Metastatic epidural spinal column compression due to pancreatic ductal adenocarcinoma causing subacute Cauda equina syndrome: A case report
Date of publication: 05-Sep-2020
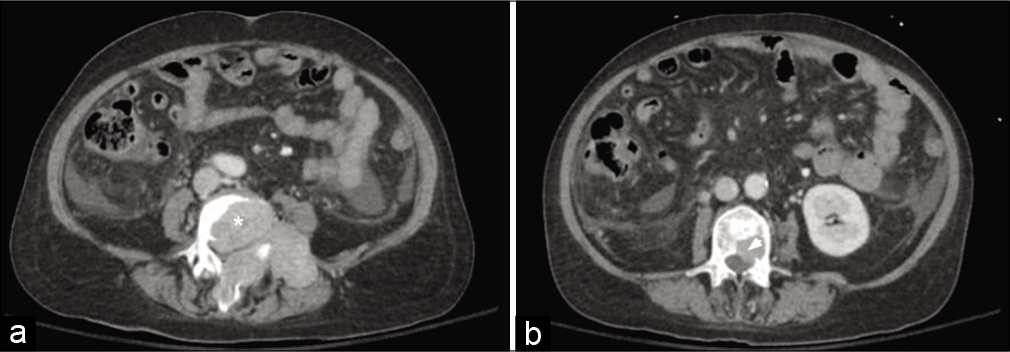
Background: Pancreatic ductal adenocarcinoma (PDAC) is the most common pancreatic malignancy, which rarely metastasizes to the spine.
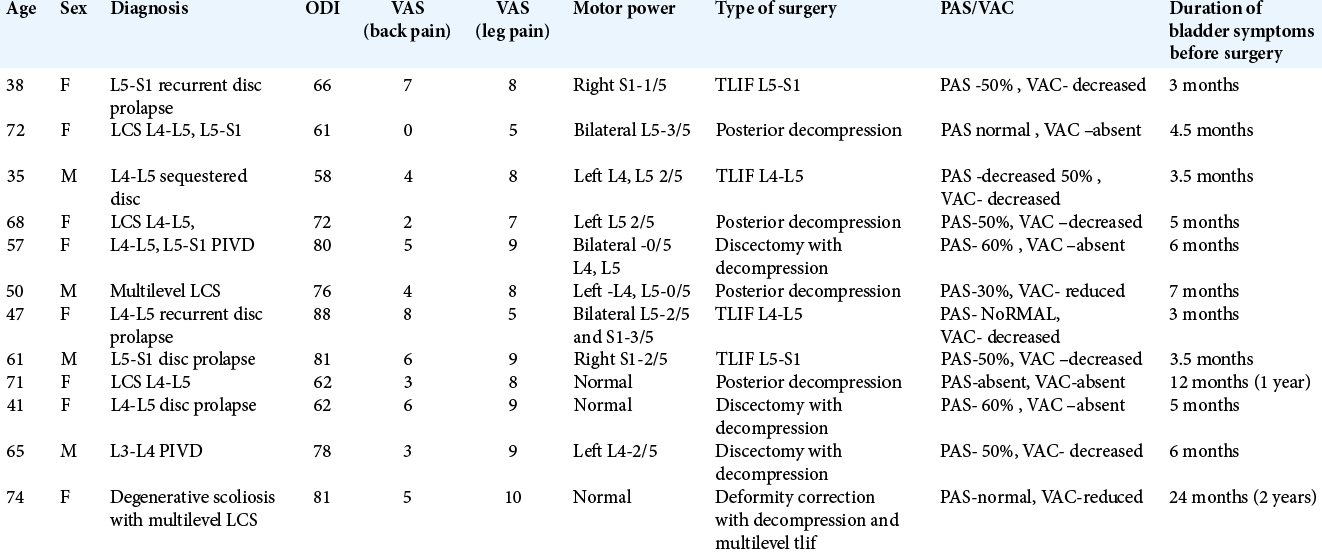
Does surgical decompression alleviate neglected cauda equina syndromes attributed to lumbar disc herniation and/or degenerative canal stenosis?
Date of publication: 05-Sep-2020
Background: Most studies recommend urgent decompression (e.g., within 48–72 h) of the symptomatic onset of a cauda equina syndrome. As patients in our area typically underwent >3 months delayed surgery for cauda equina syndromes due to disc disease/stenosis, we asked whether surgery was still worthwhile.
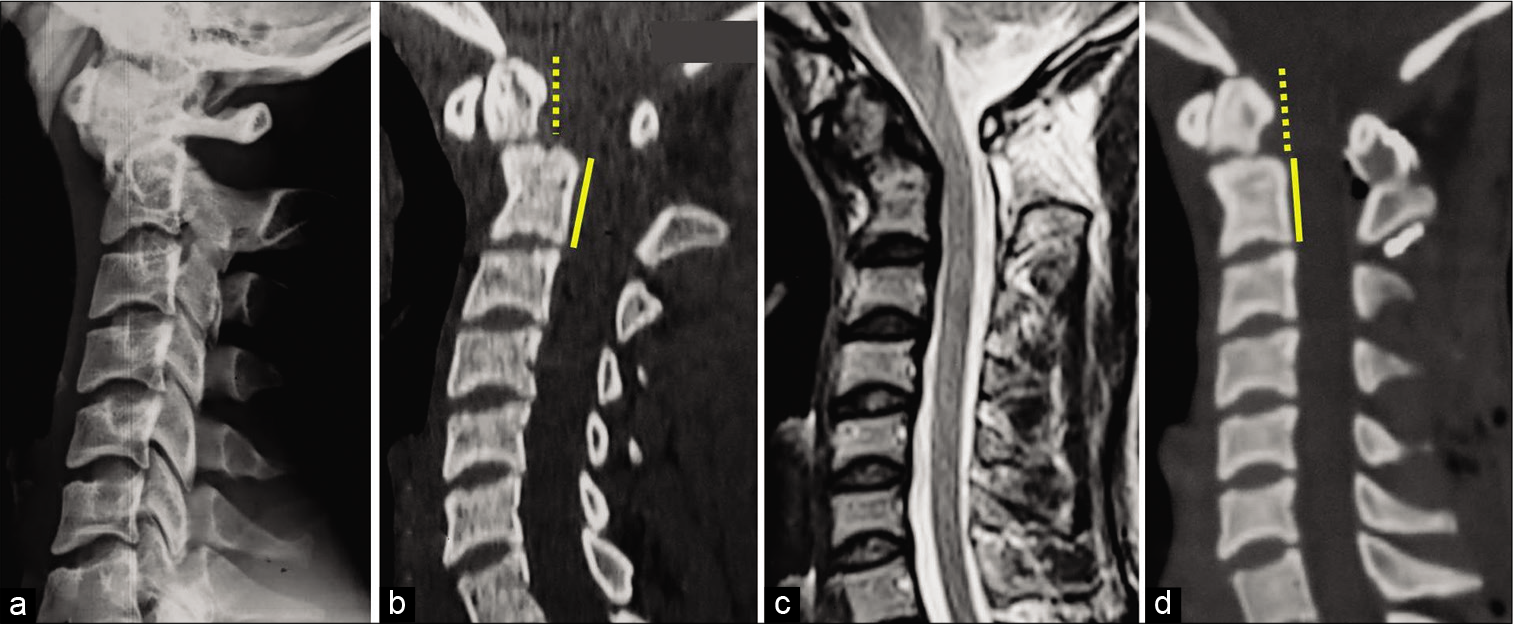
Unilateral blindness following superior laryngeal nerve block for awake tracheal intubation in a case of posterior cervical spine surgery
Date of publication: 05-Sep-2020
Background: Superior laryngeal nerve block (SUPLANEB) is a popular airway anesthesia technique utilized for successful awake endotracheal intubation in patients with significant cervical spine instability. If not performed by an expert, it carries the risk of general/neurologic complications that are typically minimal/transient. However, permanent blindness and/or upper cranial nerve neuropathies may occur. Here, we describe a case in which a young patient underwent an atlantoaxial fusion for a C2 nonunion (e.g., following a fracture) complicated by unilateral blindness due to a SUPLANEB.
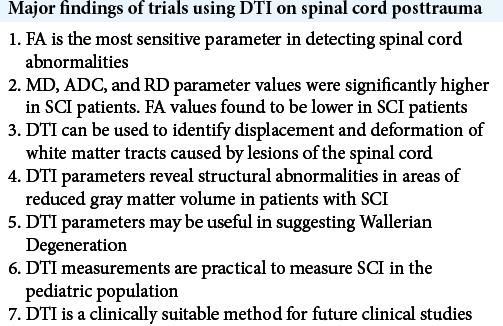
Diffusion tensor imaging of the spinal cord status post trauma
Date of publication: 05-Sep-2020
Background: Since its development in 1994, diffusion tensor imaging (DTI) has been successfully used to assess structural and functional changes to neurological tissue within the central nervous system. Namely, DTI is a noninvasive magnetic resonance imaging (MRI)-based technique that uses anisotropic diffusion to visualize and estimate the organization of white matter in neuronal tissue. It has been used to study various spinal pathologies including neoplastic diseases, degenerative myelopathy, demyelinating diseases, and infections involving the spinal cord. However, due to technical uncertainties and experimental limitations, DTI has rarely been clinically applied to assess trauma-related spinal pathologies.
Intramedullary spinal cord cavernous malformations in the pediatric population
Date of publication: 05-Sep-2020
Background: Intramedullary spinal cavernous malformations (ISCM) account for just 1% of all intramedullary pediatric spinal cord lesions. Pathologically, they are well-circumscribed vascular malformations that typically appear dark blue or reddish-brown, often coming to the spinal cord surface. With regard to the histopathology findings, ISCMs are comprised sinusoidal vascular spaces lined by a single layer of endothelial cells within a loose connective tissue stroma. As these lesions are often misdiagnosed in the pediatric population, appropriate treatment may be unduly delayed.
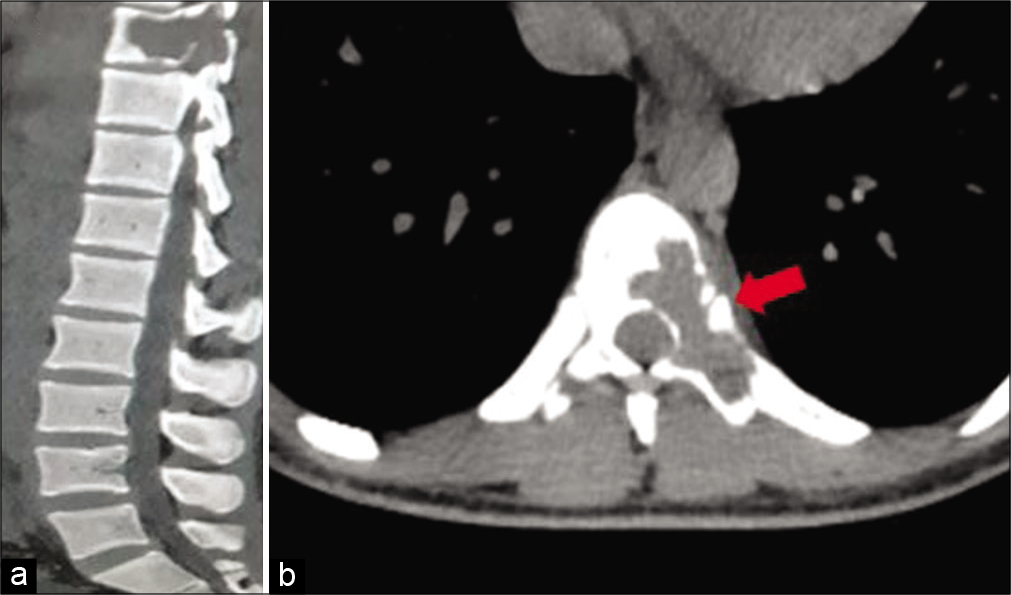
Aneurysmal bone cyst of thoracic spine with neurological deficit and its recurrence treated with multimodal intervention – A case report
Date of publication: 05-Sep-2020
Background: Aneurysmal bone cysts (ABCs) are rare, representing about 1% of primary bone tumors, and 15% of all primary spine/sacral tumors. Notably, when they are located in poorly accessible regions such as the spine and pelvis, their management may be challenging. Treatment options include selective arterial embolization (SAE), curettage, en bloc excision with reconstruction, and radiotherapy.
Comment regarding the article “Comparative metrics of neurosurgical scientific journals: What do they mean to readers?”
Date of publication: 05-Sep-2020
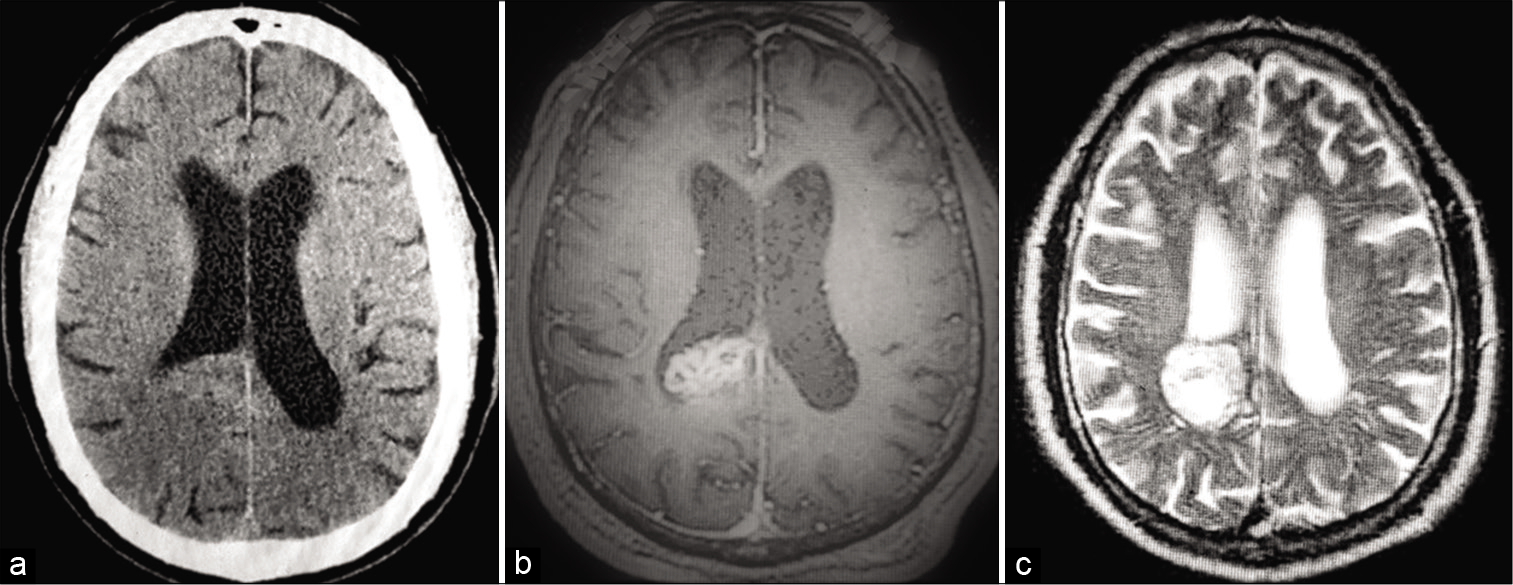
Long-term follow-up of lateral ventricular central neurocytoma treated with subtotal resection followed by concurrent chemoradiotherapy and add on chemotherapy – Case report from a Tertiary Kenyan Cancer Hospital
Date of publication: 05-Sep-2020
Background: Central neurocytomas are rare, mostly benign neuroectodermal tumors of the central nervous system typically located within the lateral and third ventricles of cerebrum. No consensus guidelines for the management of central neurocytoma available due to the rarity of the disease.
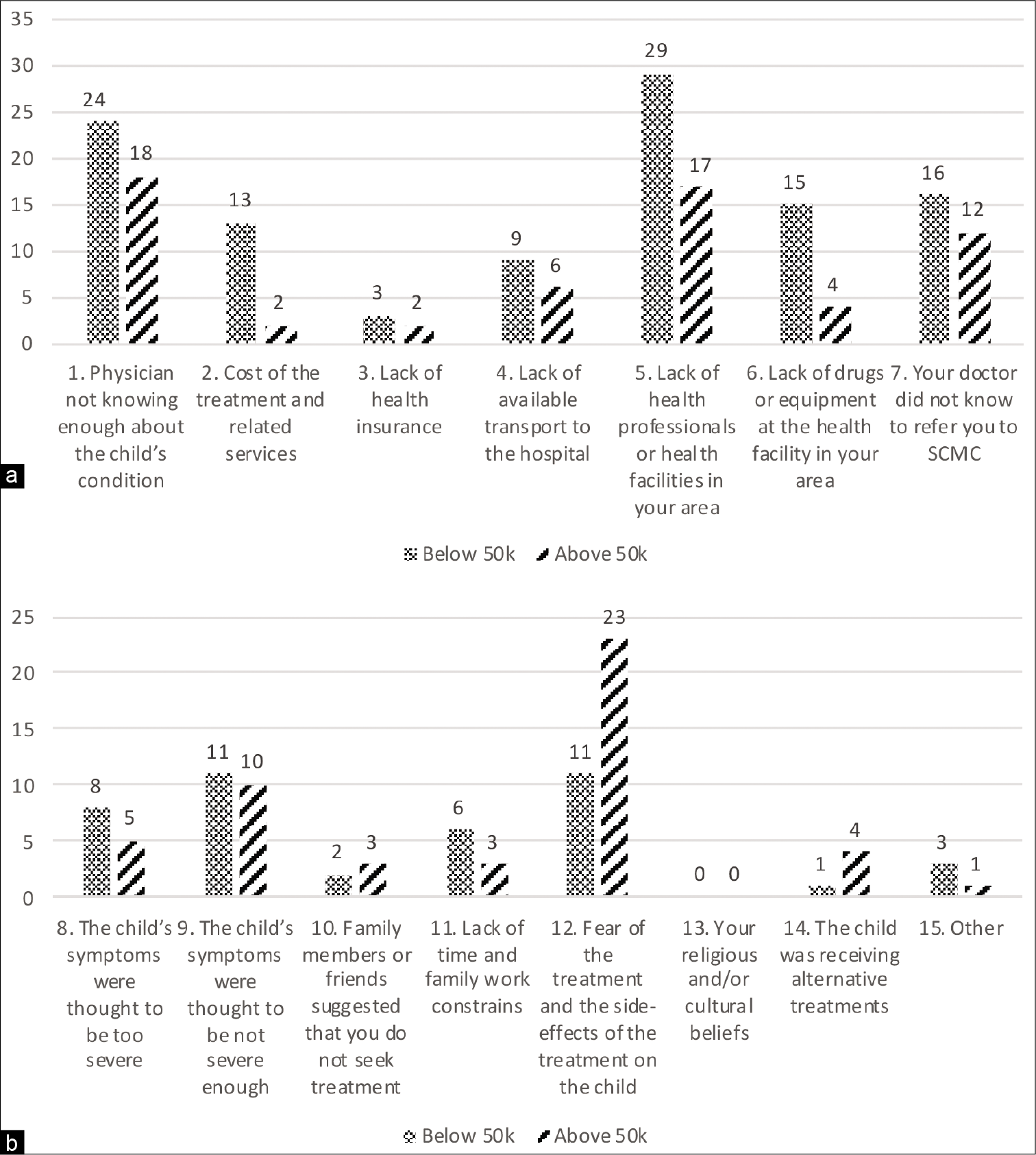
Effects of parental level of income and visual presentation of spina bifida occulta in decision making process
Date of publication: 05-Sep-2020
Background: Parents are active participants in the referral process of children with non-life-threatening surgical pathologies. Nonetheless, there is scarce literature about the influence of parent’s level of income and perception of their children’s conditions on their decision process. Our study aims at expanding our knowledge about this parameter. We focused our research on parents of children spina bifida occulta (SBO), a condition that with a broad clinical impact and that often requires timely referral.
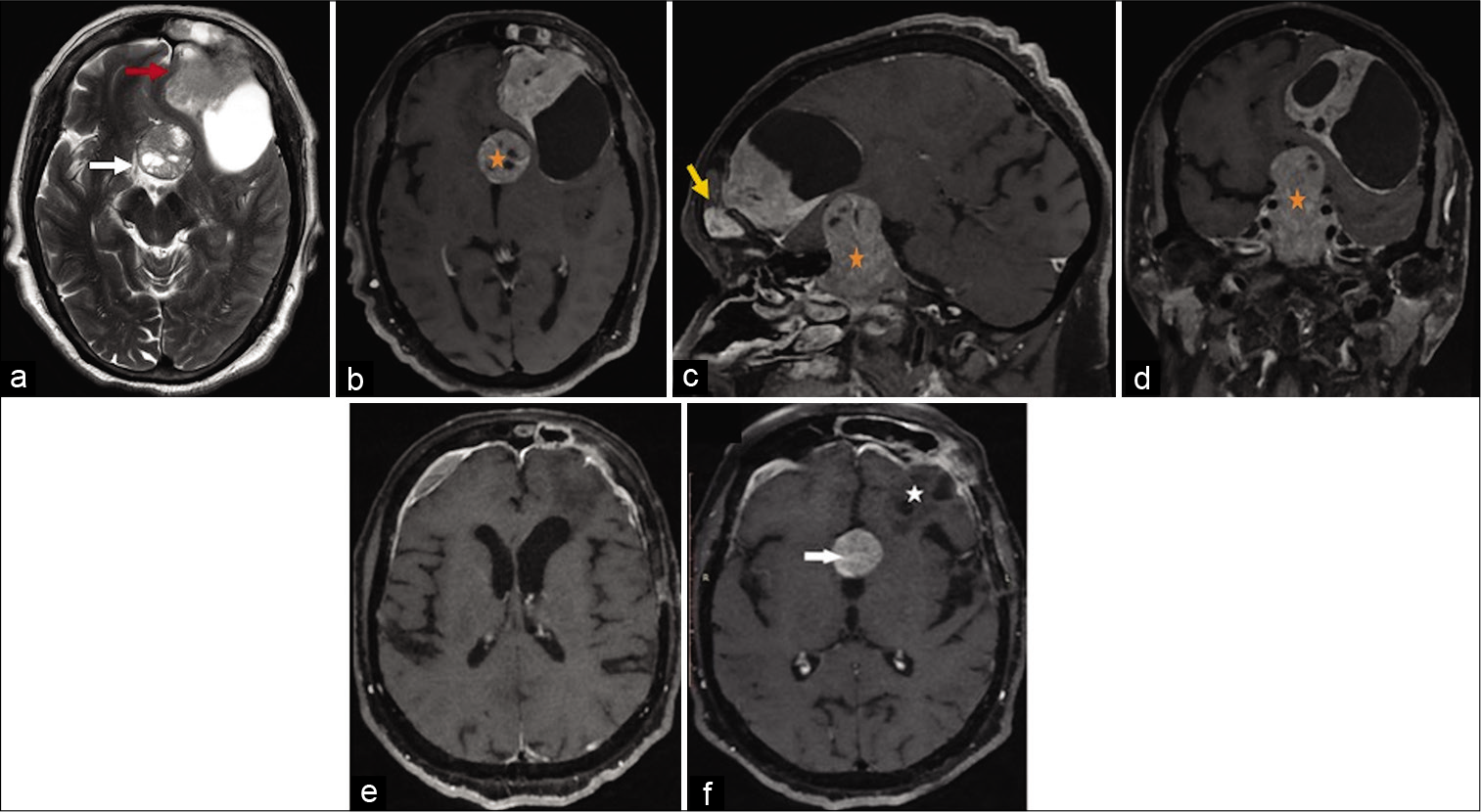
Coexistent pituitary adenoma and frontal convexity meningioma with frontal sinus invasion: A rare association
Date of publication: 05-Sep-2020
Abstract
The coexistence of pituitary adenoma (PA) and meningioma in the same patient is rare, after excluding radiotherapy-induced meningiomas. Most of the literature on their coexistence describes meningiomas located in the close vicinity to PA, that is, in the sellar/parasellar region. We describe a case of a 65-year-old lady with a nonfunctioning PA and an associated frontal convexity meningioma with frontal sinus invasion. The imaging was nonspecific for the meningioma, and its association with concomitant PA has not been reported before.