“Whiplash” cervical trauma with fracture and migration of carotid stent fragments
Date of publication: 08-Oct-2020
Background: Angioplasty using a carotid stent is a treatment modality for carotid stenosis, with results similar to those obtained with endarterectomy, as demonstrated by important studies. The increasing use of this procedure has also led to a larger number of reports of complications, stent fractures among those. Stent fracture is a rare manifestation and hence needs further studying so that its actual prevalence can be determined, as well as its associated risk factors and proper clinical management. The current study reports the case of a patient who had previously undergone angioplasty with a carotid stent and, after an automobile accident, presented with a stent fracture and distal embolization of fragments thereof with neurological manifestation.
Fusiform superior cerebellar artery aneurysm treated with flow diversion: A case report
Date of publication: 08-Oct-2020
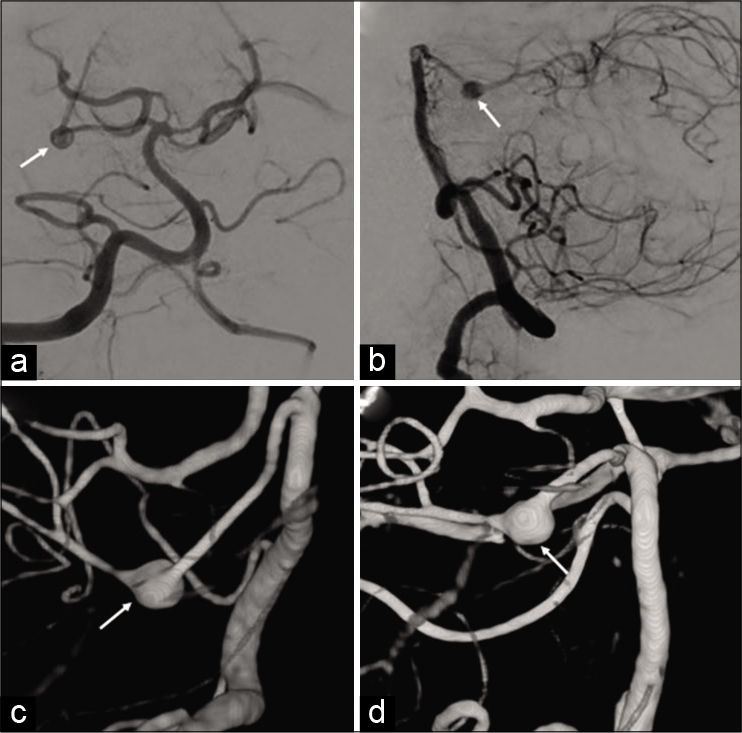
Background: Fusiform aneurysms of the distal superior cerebellar artery are rare and challenging to treat. Due to the rarity of these lesions, there is little consensus regarding their management. Treatment options have traditionally included parent artery sacrifice with either an endovascular approach or microsurgical clipping. Given the small diameter of the superior cerebellar artery, flow diversion has not been typically considered as a viable treatment option for these aneurysms.
Lumbosacral extradural extramedullary hematopoiesis in thalassemia major causing spinal canal stenosis
Date of publication: 08-Oct-2020
Background: Extramedullary hematopoiesis (EH) is common in patients with ineffective erythropoiesis like thalassemia major (TM). EH commonly involves intra-abdominal organs (e.g., spleen and liver), but rarely involves vertebral bodies. Here, we reviewed images of EH contributing to spinal canal stenosis.
Case report (precis): Atypical delayed presentation of cervical spinal epidural abscess
Date of publication: 08-Oct-2020
Background: Older patients with spinal epidural abscesses (SEA) may present in an atypical fashion, failing to exhibit the classical triad of pain, fever, and a neurological deficit. Rather, they may be less aware of pain, fail to develop a fever, and attribute their neurological deficit to “old age.” Further, their laboratory studies may not be abnormal, and critical findings on MR (i.e., more so than CT studies) may be overlooked. Here, we present an elderly patient with severe upper extremity monoparesis whose cervical SEA was overlooked for months.
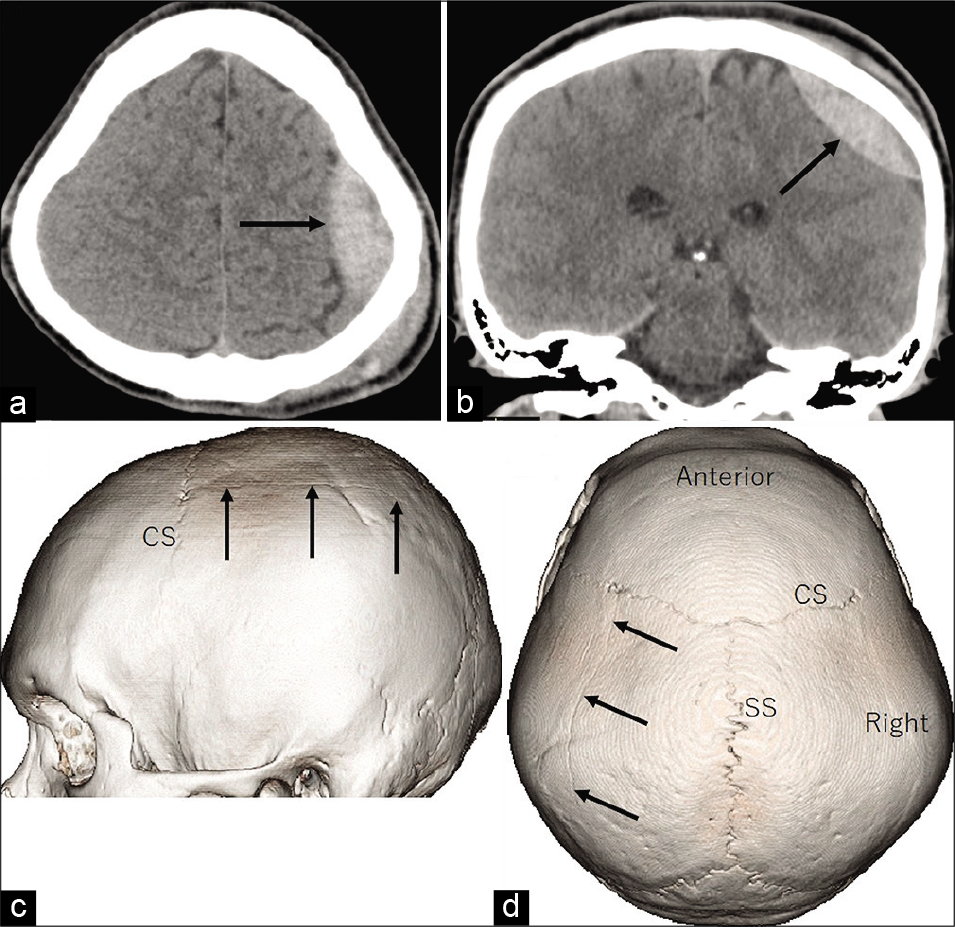
Traumatic acute epidural hematoma caused by injury of the diploic channels
Date of publication: 08-Oct-2020
Background: Traumatic acute epidural hematomas (EDHs) commonly develop by rupture of the meningeal arteries. EDH caused by an injury of the diploic channel (DC) has not been reported.
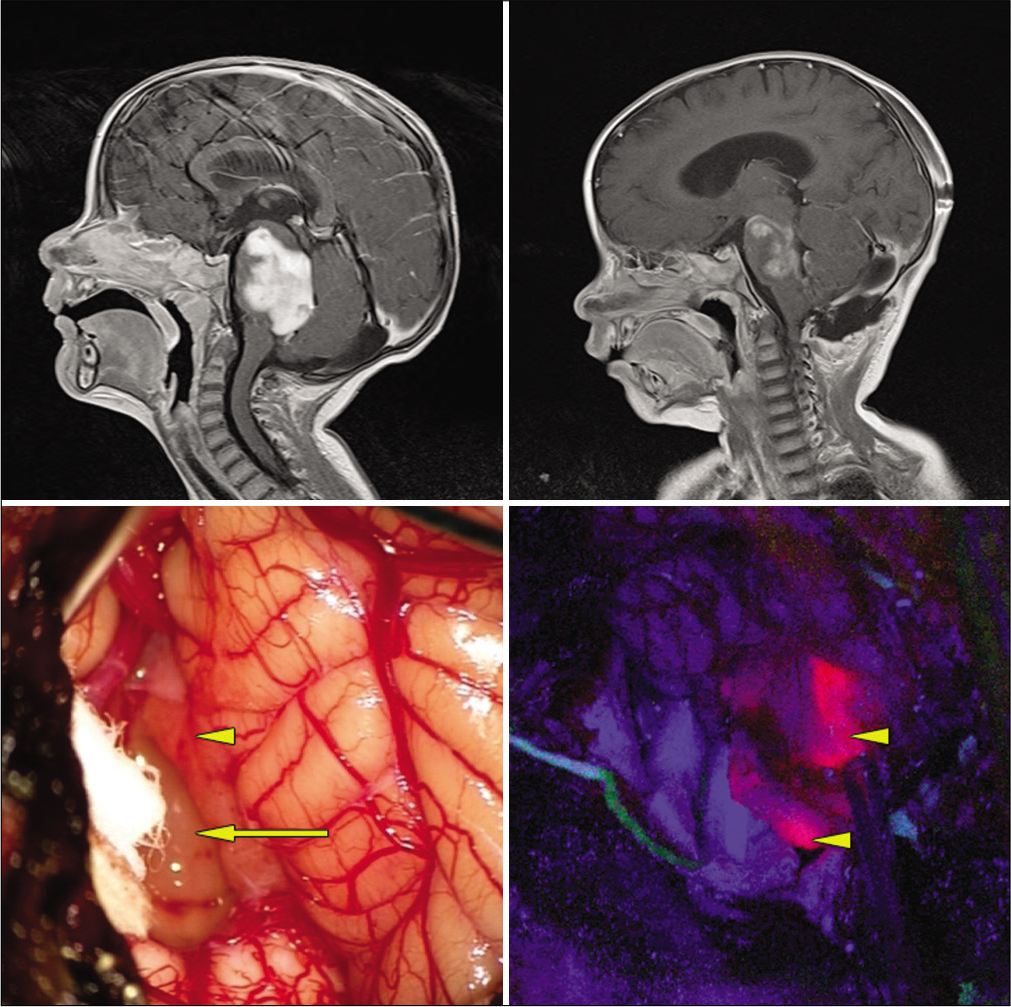
5-aminolevulinic acid-guided surgery for focal pediatric brainstem gliomas: A preliminary study
Date of publication: 08-Oct-2020
Background: There is a growing body of literature supporting the use of 5-aminolevulinic acid (5-ALA) in the pediatric population, however, its use is still considered “off label” in this setting. In this retrospective study, we report our experience using 5-ALA in pediatric patients with focal brainstem gliomas (BSGs).
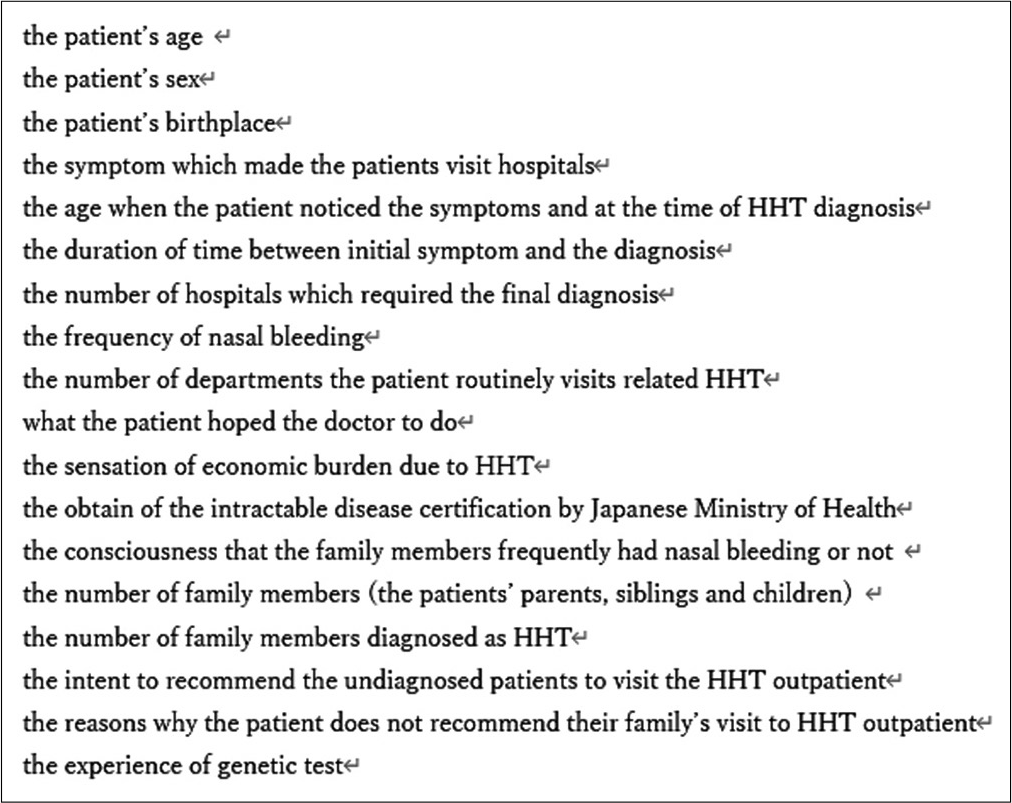
A questionnaire-based survey to evaluate and improve the current HHT medical and social condition in Japan
Date of publication: 02-Oct-2020
Background: Hereditary hemorrhagic telangiectasia (HHT) is a genetic systemic vascular disease affecting multiple organs and shows recurrent intractable symptoms. This disease has not been widely recognized in Japan until recently. Both diagnosed HHT patients and potential ones have faced difficulties because of the unfamiliarity with the disease in Japan. To evaluate the effect and degree of such a Japanese situation, a questionnaire-based survey was executed in this study.
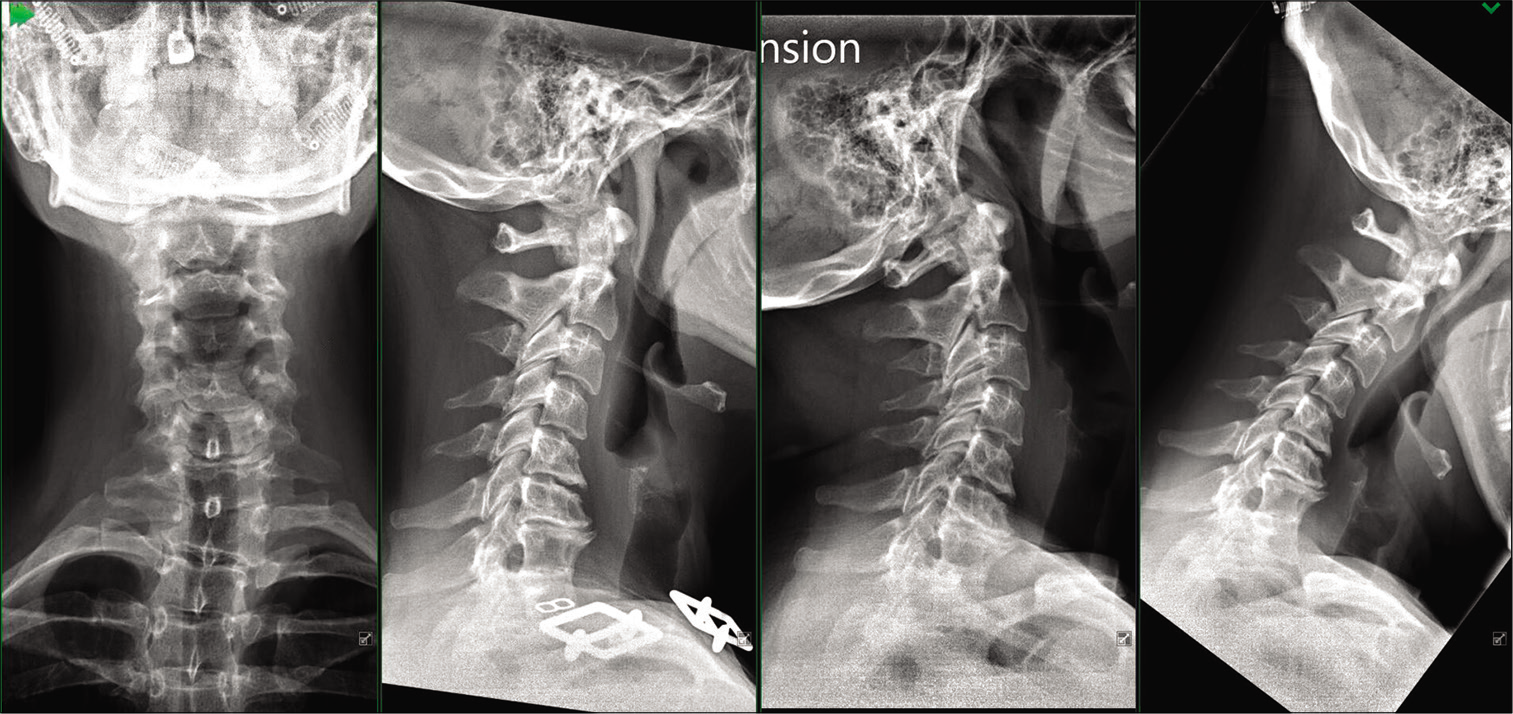
Two-level cervical disc arthroplasty in patients with Klippel-Feil syndrome: A case report and review of the literature
Date of publication: 02-Oct-2020
Background: Klippel-Feil syndrome (KFS) is defined by multiple abnormal segments of the cervical spine with congenital synostosis of two or more cervical vertebrae. KFS patients who demonstrate progressive symptomatic instability and/or neurologic sequelae are traditionally managed with operative decompression and arthrodesis.
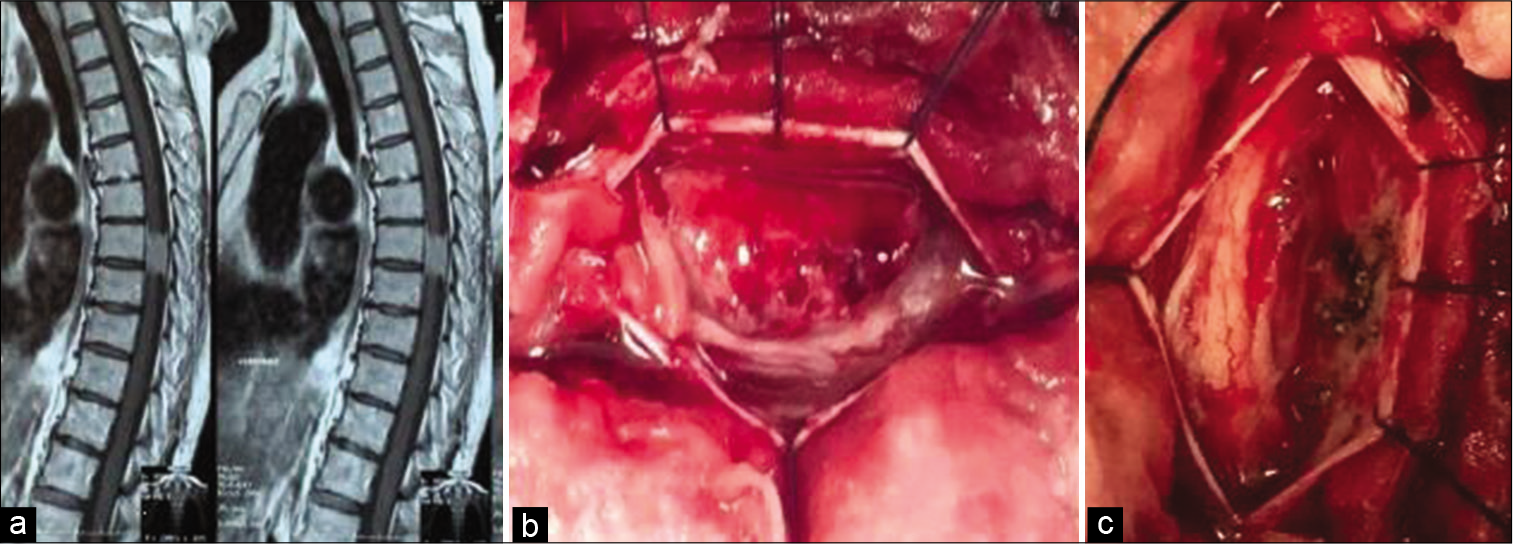
Delayed recovery from paraplegia following resections of thoracic meningiomas
Date of publication: 02-Oct-2020
Background: In this retrospective study, we evaluated the patterns of postoperative recovery for patients who were initially paraplegic before the excision of thoracic spine meningiomas. We also determined how the various prognostic factors impacted outcomes.
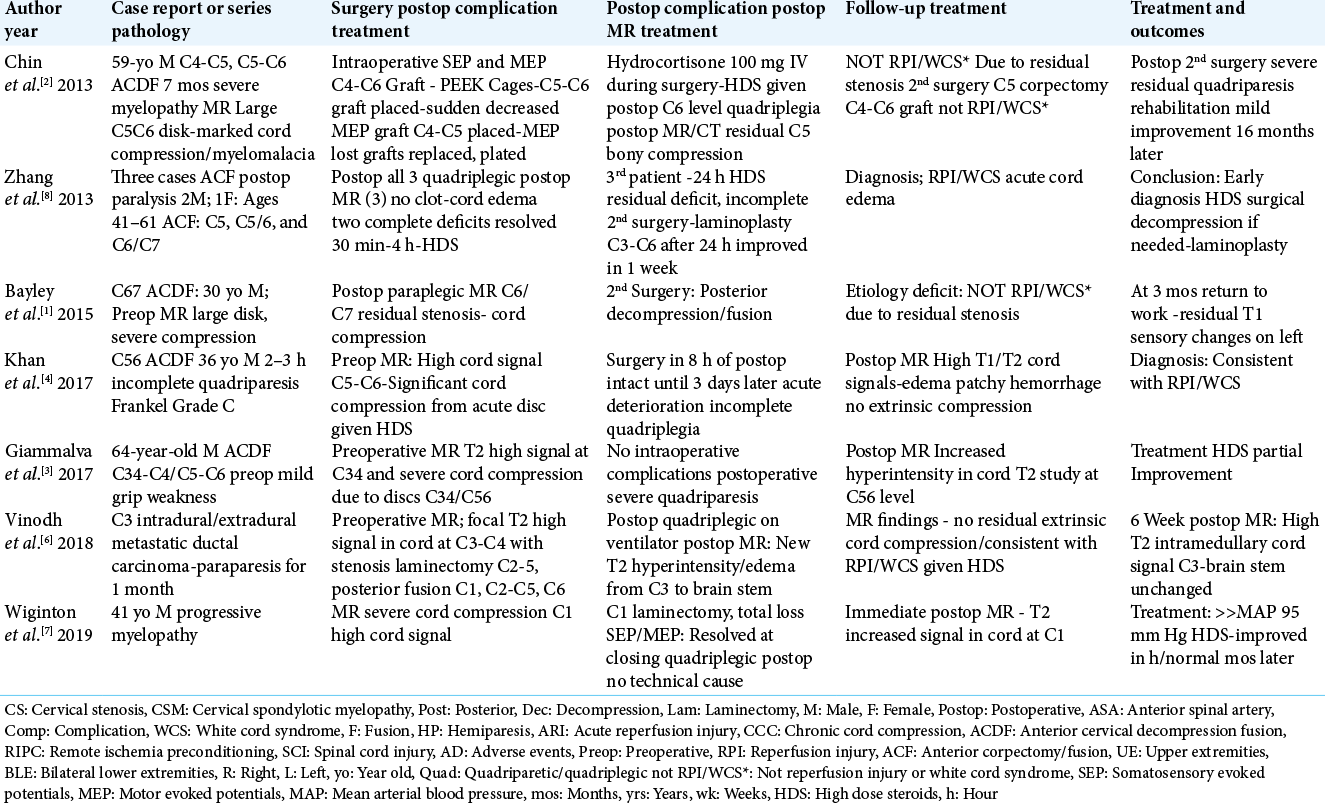
Reperfusion Injury (RPI)/White Cord Syndrome (WCS) Due to Cervical Spine Surgery: A Diagnosis of Exclusion
Date of publication: 02-Oct-2020
Background: Following acute cervical spinal cord decompression, a subset of patients may develop acute postoperative paralysis due to Reperfusion Injury (RPI)/White Cord Syndrome (WCS). Pathophysiologically, this occurs due to the immediate restoration of normal blood flow to previously markedly compressed, and under-perfused/ischemic cord tissues. On emergent postoperative MR scans, the classical findings for RPI/ WCS include new or expanded, and focal or diffuse intramedullary hyperintense cord signals consistent with edema/ischemia, swelling, and/or intrinsic hematoma. To confirm RPI/WCS, MR studies must exclude extrinsic cord pathology (e.g. extramedullary hematomas, new/residual compressive disease, new graft/vertebral fracture etc.) that may warrant additional cervical surgery to avoid permanent neurological sequelae.