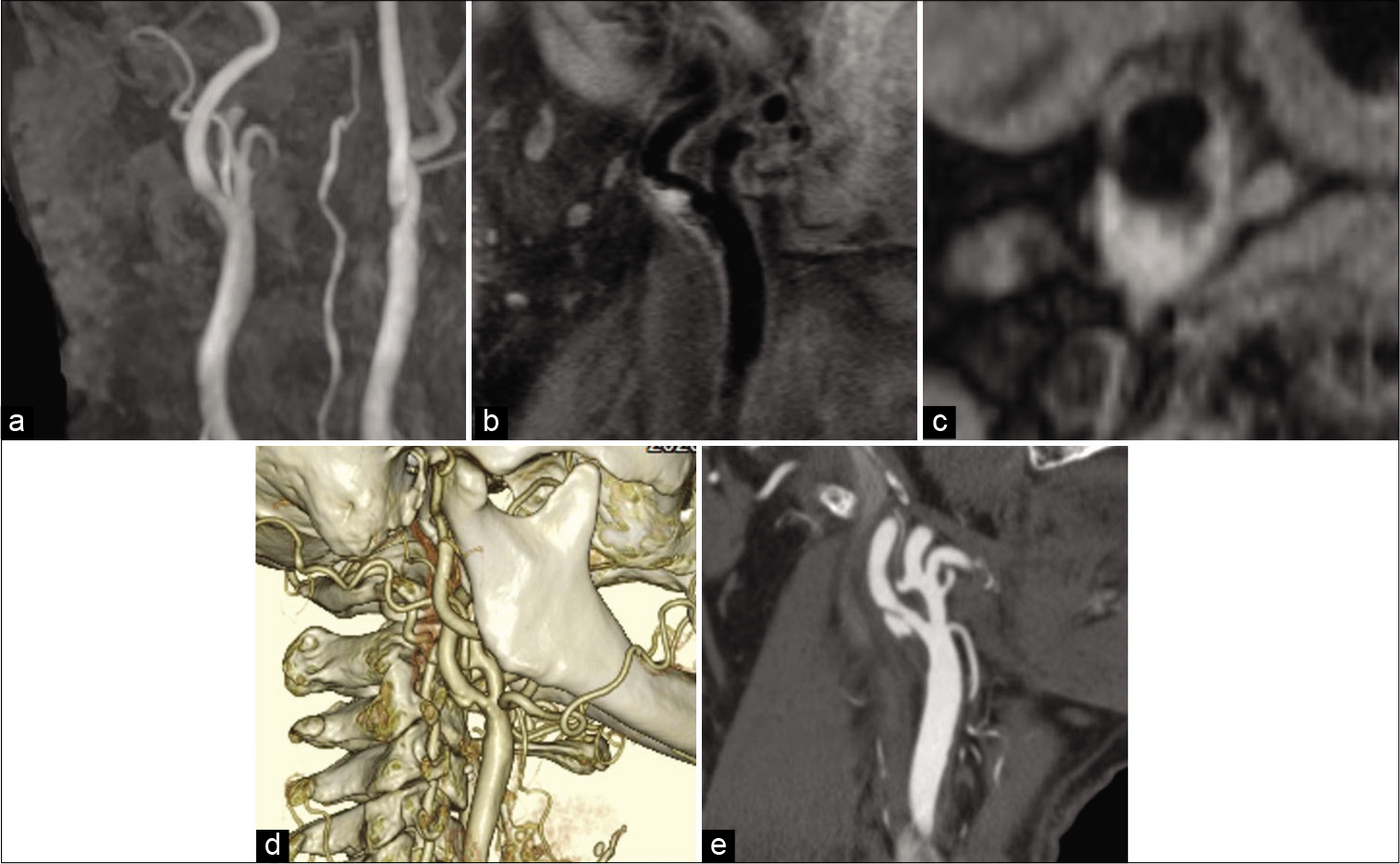
Unusual course of the vagus nerve passing anterior to the internal carotid artery during carotid endarterectomy
Date of publication: 14-Jun-2021
Background: Carotid endarterectomy (CEA) is a conventional surgical technique to prevent ischemic stroke and the effectiveness for advanced lesions is established in many large studies. The vagus nerve is one of the cranial nerves that we usually encounter during CEA manipulation, which is identified as located posterior to the vessels in a position posterolateral to the carotid artery and posteromedial to the internal jugular vein.
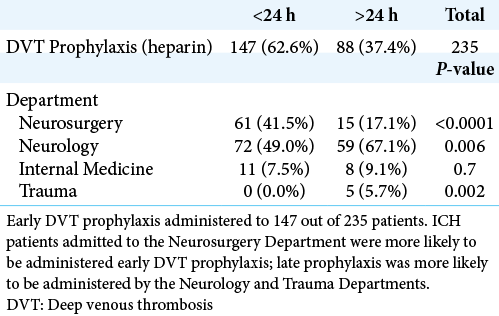
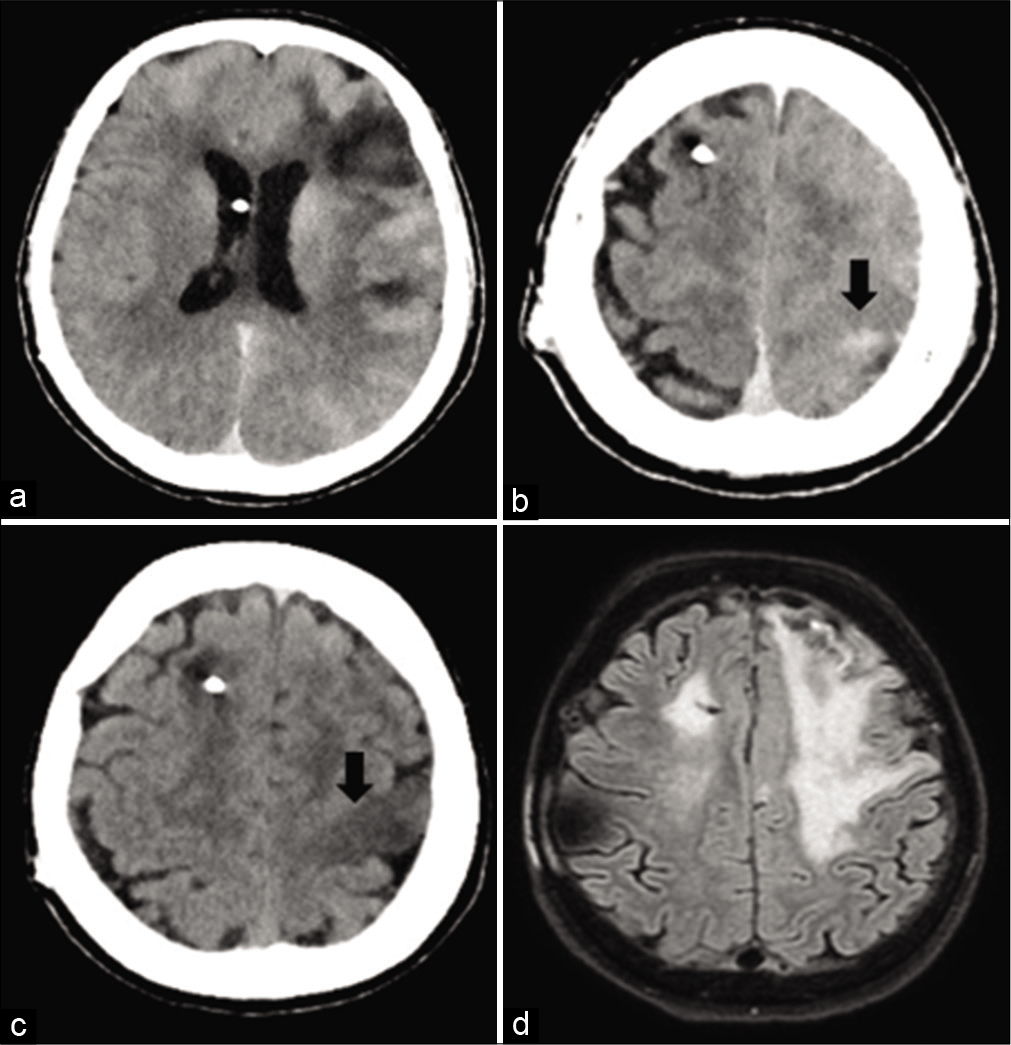
Early chemoprophylaxis for deep venous thrombosis does not increase the risk of hematoma expansion in patients presenting with spontaneous intracerebral hemorrhage
Date of publication: 14-Jun-2021
Background: Spontaneous intracerebral hemorrhage (ICH) is a significant cause of morbidity and mortality worldwide. The development of venous thromboembolism (VTE), including deep venous thrombosis or pulmonary embolism, is correlated with negative outcomes following ICH. Due to the risk of hematoma expansion associated with the use of VTE chemoprophylaxis, there remains significant debate about the optimal timing for its initiation following ICH. We analyzed the risk of early chemoprophylaxis on hematoma expansion following ICH.
Use of Saito technique to resect an anterior lumbar spine meningioma: Technical note
Date of publication: 14-Jun-2021
Background: Complete (Simpson Grade I: total removal) resections for anterior spinal meningiomas are especially challenging. This is largely attributed to difficulty obtaining a water-tight dural repair where the tumor has infiltrated the dura requiring duroplasty, thus often resulting in just a Simpson Grade II resection (i.e. coagulation of the dural implantation site). Here, we present a 56-year-old female who underwent resection of a ventral lumbar meningioma utilizing the Saito technique, that effectively separated the dura into two layers, removing just the inner layer but leaving the outer layer intact for direct dural repair.
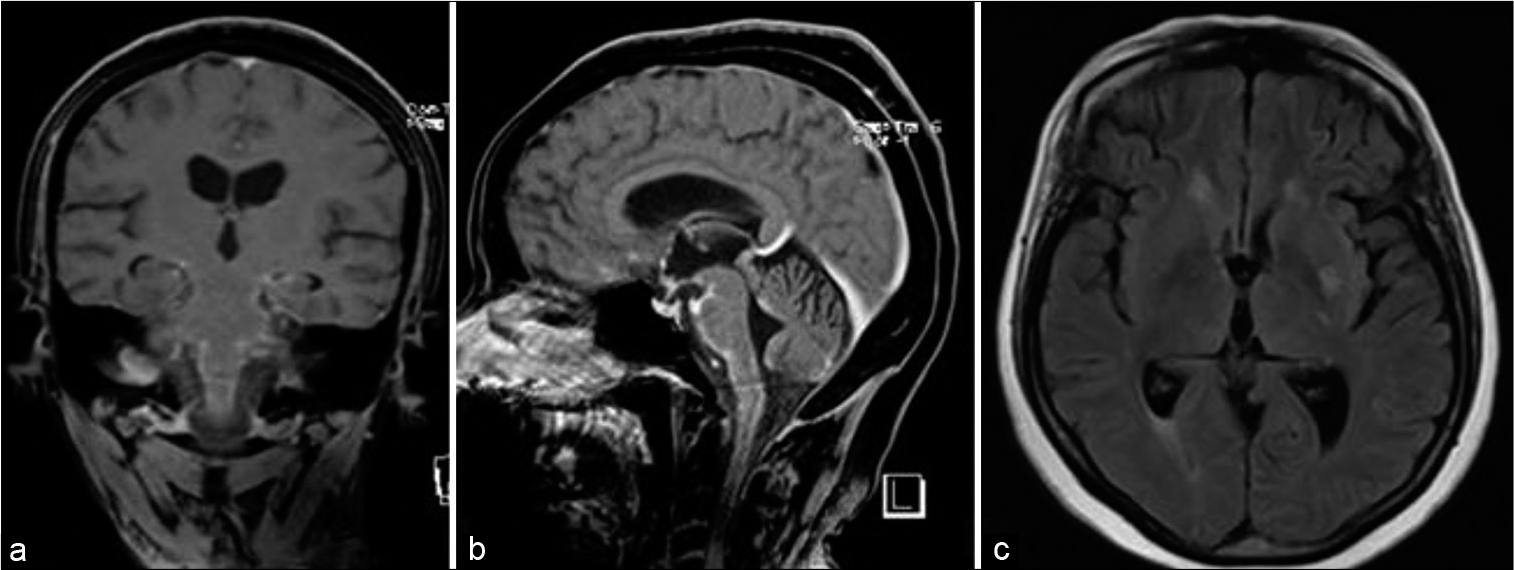
Spinal intramedullary abscess due to Candida albicans in an immunocompetent patient: A rare case report
Date of publication: 14-Jun-2021
Background: A spinal intramedullary abscess is a rare clinical entity in which patients classically present with a subacute myelopathy and progressive paraplegia, sensory deficits, and/or bowel and bladder dysfunction. We report the second case of spinal intramedullary abscess caused by Candida albicans to ever be published and the first case of its kind to be surgically managed.
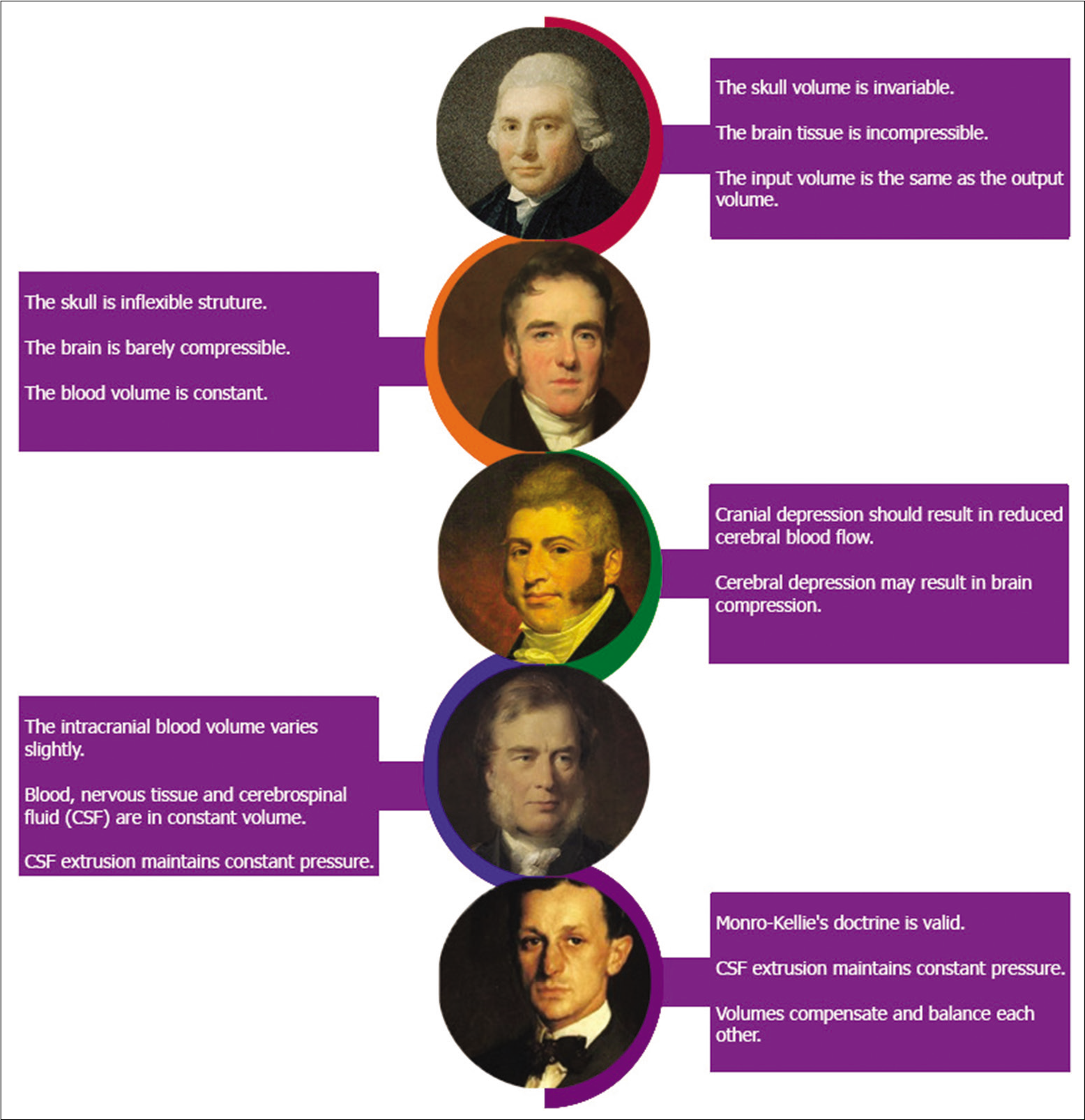
The historic evolution of intracranial pressure and cerebrospinal fluid pulse pressure concepts: Two centuries of challenges
Date of publication: 14-Jun-2021
Background: There is a consensus on the importance of monitoring intracranial pressure (ICP) during neurosurgery, and this monitoring reduces mortality during procedures. Current knowledge of ICP and cerebrospinal fluid pulse pressure has been built thanks to more than two centuries of research on brain dynamics.
Contrast-induced encephalopathy and permanent neurological deficit: A case report and literature review
Date of publication: 14-Jun-2021
Background: Contrast-induced encephalopathy (CIE) is a rare condition that occurs after intravenous or intra-arterial contrast agent administration. Patients generally show different ranges of neurological deficits, which generally resolve themselves spontaneously within 24–48 h or in rare cases within 2 weeks.
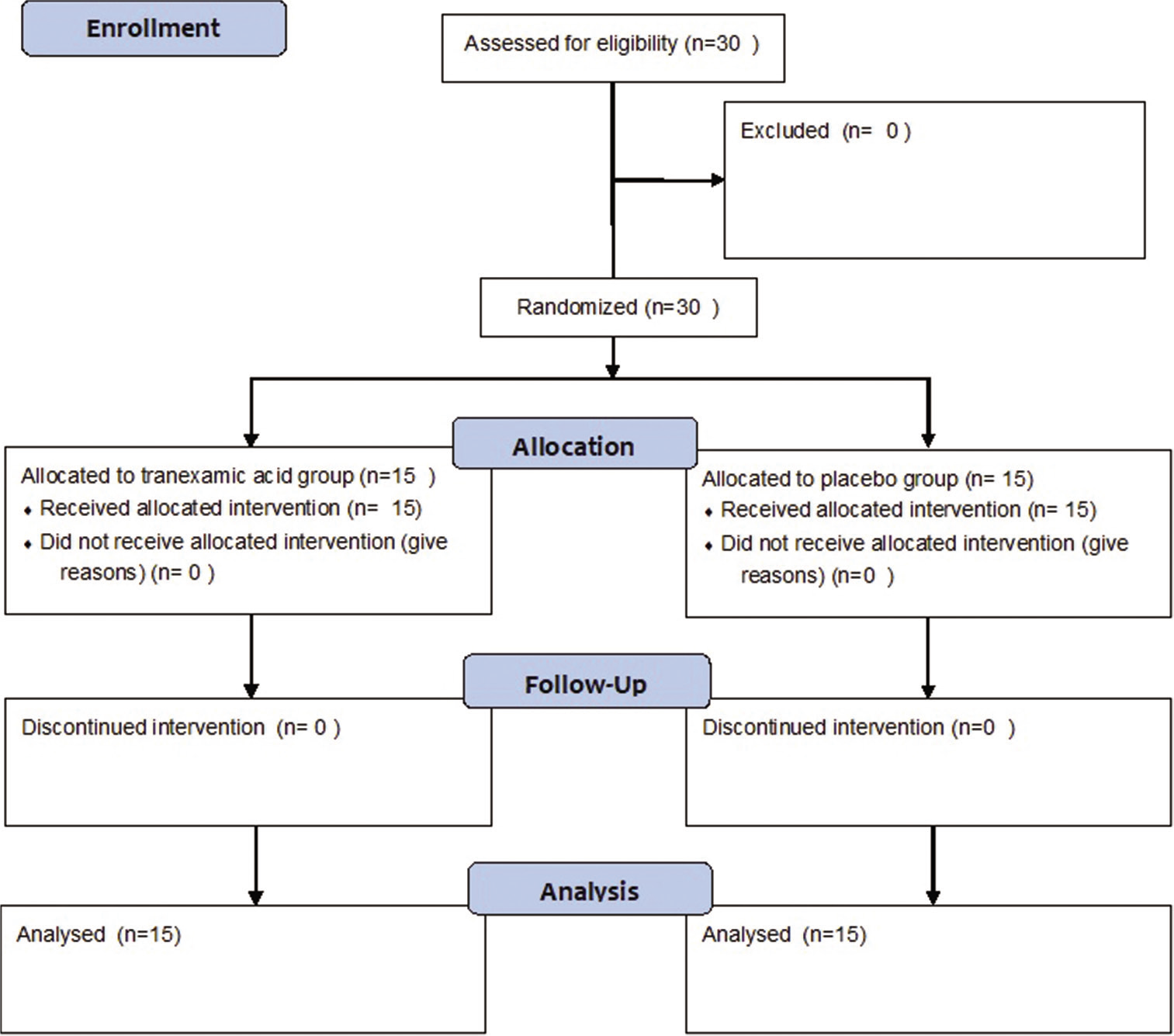
Effect of tranexamic acid on blood loss, coagulation profile, and quality of surgical field in intracranial meningioma resection: A prospective randomized, double-blind, placebo-controlled study
Date of publication: 07-Jun-2021
Background: Resection of intracranial meningioma has been associated with significant blood loss. Providing a clear surgical field and maintaining hemodynamic stability are the major goals of anesthesia during meningioma surgery. Tranexamic acid has been used to reduce blood loss in various neurosurgical settings with limited evidence in literature. A randomized, double-blind, and placebo-controlled trial was conducted to evaluate the efficacy of tranexamic acid on blood loss, coagulation profile, and quality of surgical field during resection of intracranial meningioma.
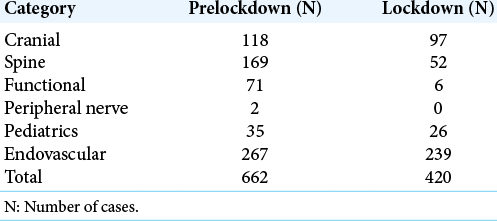
The effect of COVID-19 on trainee operative experience at a multihospital academic neurosurgical practice: A first look at case numbers
Date of publication: 07-Jun-2021
Background: COVID-19 has had a significant impact on the economy, health care, and society as a whole. To prevent the spread of infection, local governments across the United States issued mandatory lockdowns and stay-at-home orders. In the surgical world, elective cases ceased to help “flatten the curve” and prevent the infection from spreading to hospital staff and patients. We explored the effect of the cancellation of these procedures on trainee operative experience at our high-volume, multihospital neurosurgical practice.
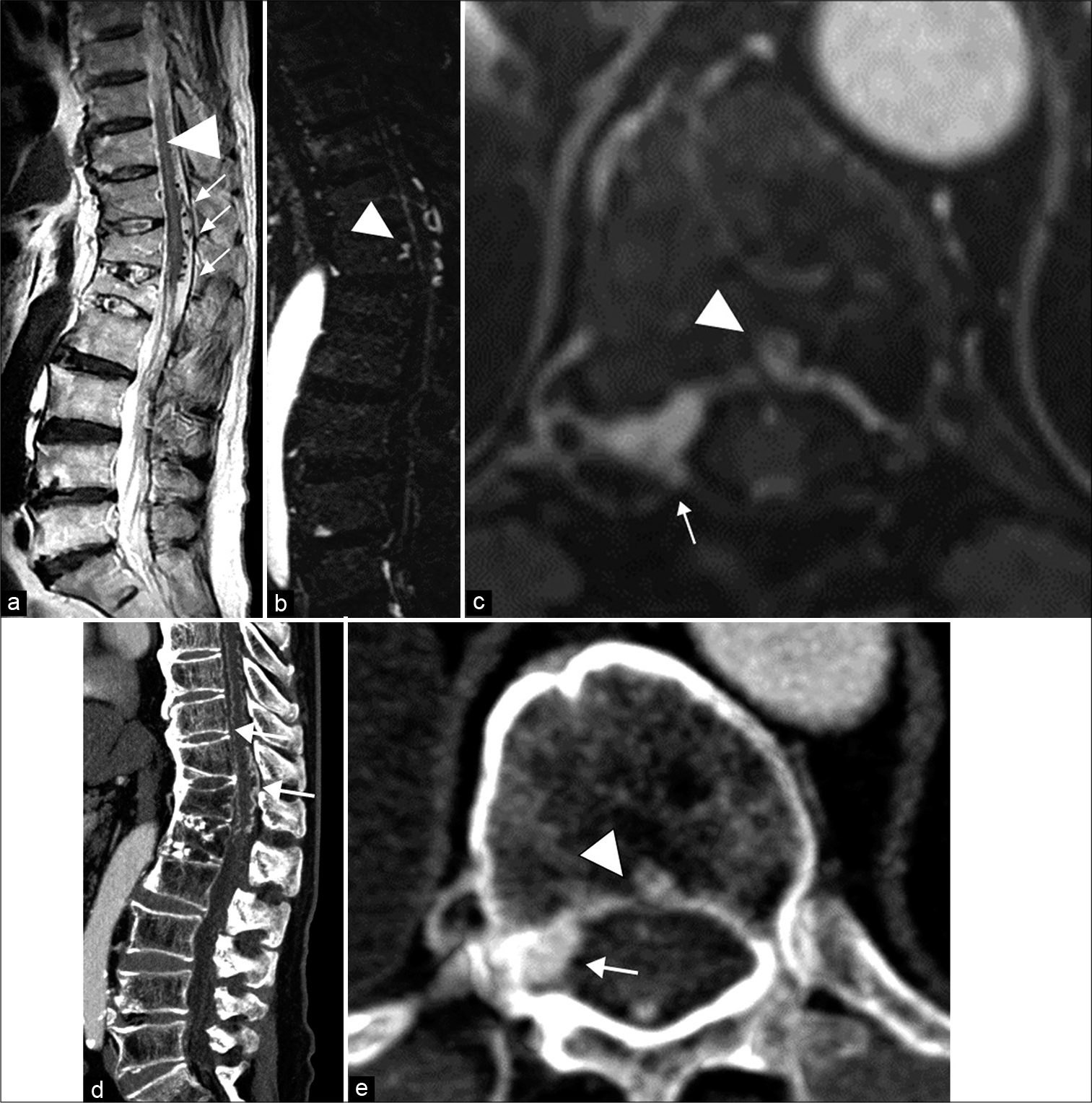
Thoracolumbar intraosseous spinal epidural arteriovenous fistulas after vertebral compression fracture: A case report and literature review
Date of publication: 07-Jun-2021
Background: The pathophysiology of spinal epidural arteriovenous fistulas (SEAVFs) with perimedullary venous drainage remains to be elucidated. This report describes a case of intraosseous SEAVF in a patient with a history of a thoracolumbar vertebral fracture at the same level 10 years before presenting with progressive myelopathy secondary to retrograde venous reflux into the perimedullary vein.
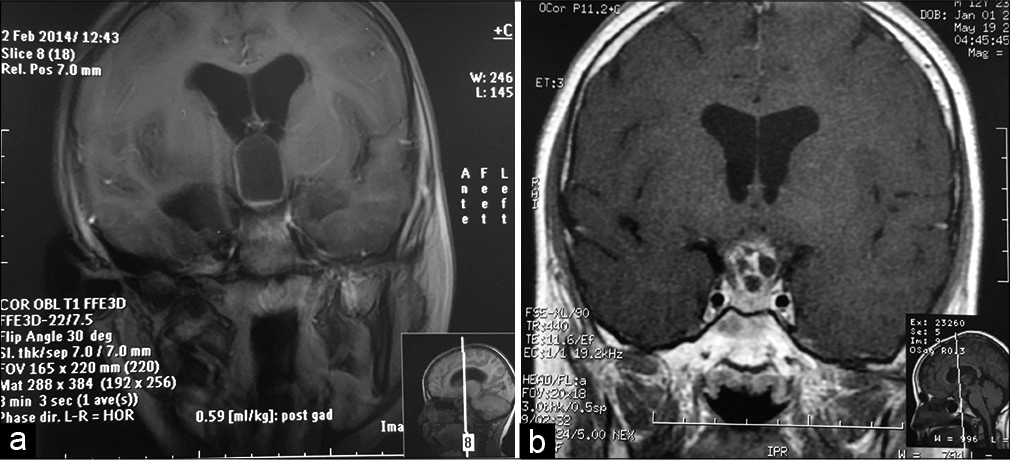
Surgical techniques in the management of supratentorial pediatric brain tumors: 10 years’ experience at a tertiary care center in the Middle East
Date of publication: 07-Jun-2021
Background: The goal of this retrospective study is to present the first epidemiological data on pediatric supratentorial central nervous system (CNS) tumors in Lebanon and to review the various surgical management strategies used.