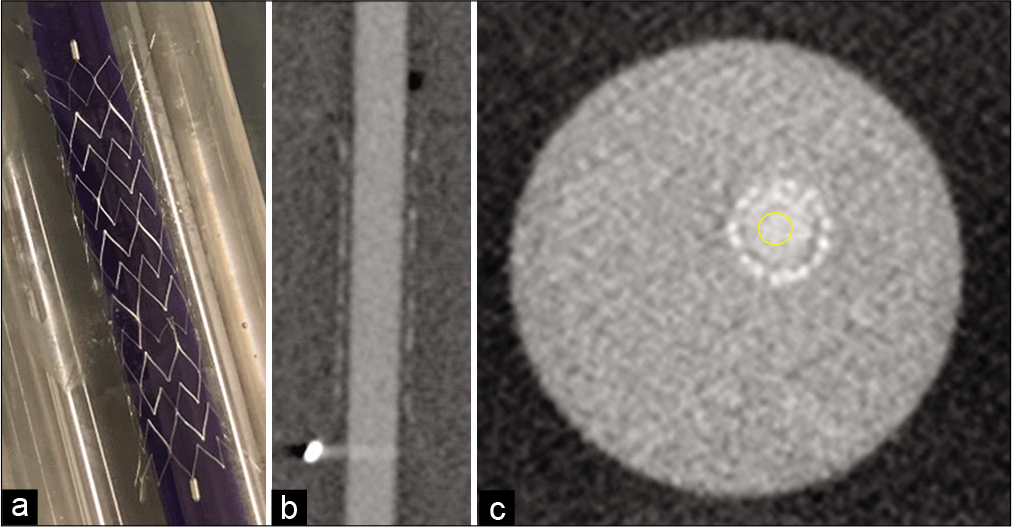
Optimum concentration of iodine contrast agent injection for best stent visualization using Neuroform Atlas stent during stent-assisted coil embolization: Case reviews based on in vitro experiments
Date of publication: 27-Jun-2020
Background: The present study aimed to evaluate the influence of contrast agent concentration (Conc) on the visibility of Neuroform Atlas in vitro and in clinical cases.
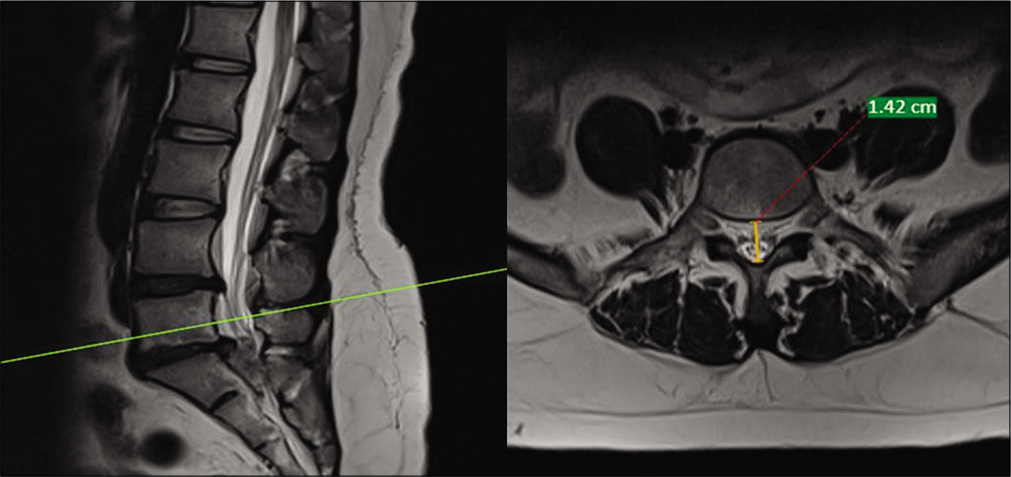
Magnetic resonance imaging findings in intervertebral disc herniation: Comparison of canal compromise and canal size in patients with and without cauda equina syndrome
Date of publication: 27-Jun-2020
Background: Surgical decompressions are typically warranted in patients with magnetic resonance (MR) and clinical evidence of cauda equina syndromes (CESs). However, it is still unclear what MR findings best correlate with such CES. Here, we compared MR-documented canal size and level/extent of compromise in 52 patients with and 56 others without CES attributed to lumbar disc herniation.
Combined Type 1 and 2 split cord malformations, kyphoscoliosis, tethered cord, and a lipoma
Date of publication: 27-Jun-2020
Background: Split cord malformations (SCMs) are uncommon congenital anomalies. They can be divided into Type 1 (bony septum and two separate dural sheaths) and Type 2 (fibrous septum and a single dural sheath).[
Comparative metrics of neurosurgical scientific journals: What do they mean to readers?
Date of publication: 27-Jun-2020
Background: In regard to scientific information, are we effectively reaching the universe of physicians in the 21st century, all of whom have different backgrounds, practice environments, educational experiences, and varying degrees of research knowledge?
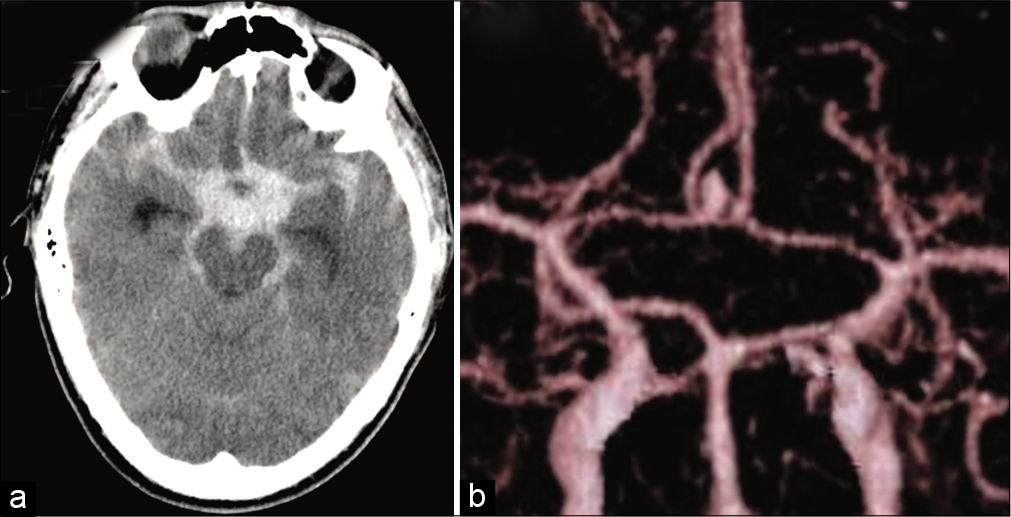
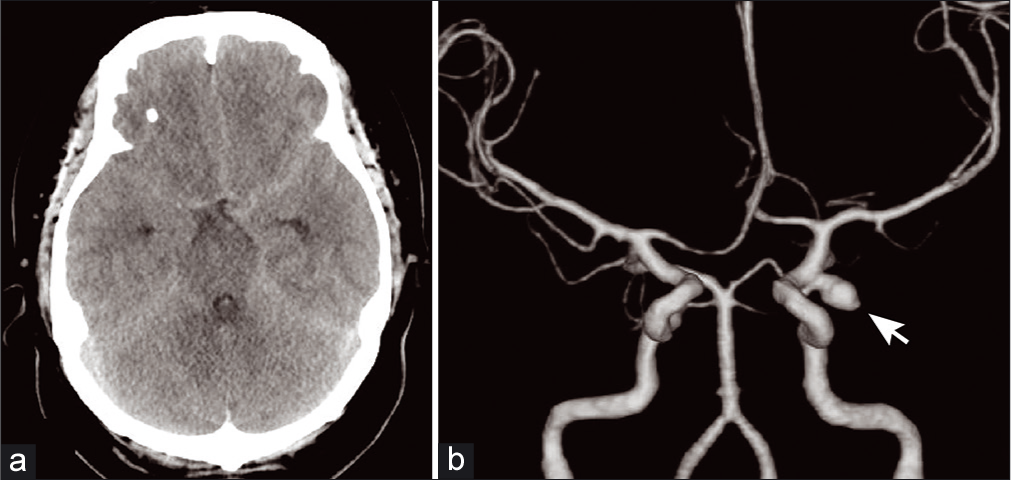
Paramedian thalamic infarction caused by cisternal drain placement in open clipping for aneurysmal subarachnoid hemorrhage: Two case reports
Date of publication: 27-Jun-2020
Background: Some complications associated with cisternal drainage have been reported; however, there are few reports on direct vascular injury caused by cisternal drain. We experienced two rare cases of thalamic infarction caused by cisternal drain placement during open clipping for a ruptured anterior communicating artery (AcomA) aneurysm through an anterior interhemispheric approach.
Management of a large intraorbital wooden foreign body: Case report
Date of publication: 20-Jun-2020
Background: Intraorbital foreign bodies are a global injury and occur with a frequency of one in six orbital injuries; however, intraorbital wooden foreign bodies are uncommon. Intraorbital wooden foreign bodies predominantly affect the male population with a mean age ranging from 21 to 22 years. The diagnosis of intraorbital wooden foreign bodies depending on their size can be challenging on imaging and if not removed early the risk of infection is high.
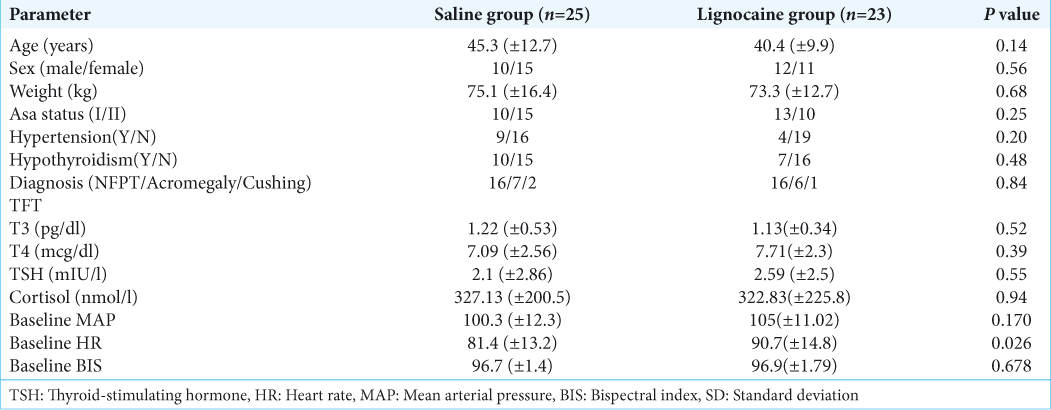
Effect of intravenous lignocaine infusion on the quality of emergence in patients undergoing transsphenoidal resection of pituitary tumors – A prospective, randomized controlled trial
Date of publication: 20-Jun-2020
Background: Emergence from anesthesia is a critical step in patients undergoing transsphenoidal pituitary surgery (TSS). The cough suppressant and anesthetic sparing properties of lignocaine makes it a favorable option for smooth extubation and maintaining stable hemodynamics intraoperatively. We aimed to evaluate the effect of lignocaine infusion on the quality of emergence (QOE) and intraoperative hemodynamics in patients undergoing transsphenoidal resection of pituitary tumors.
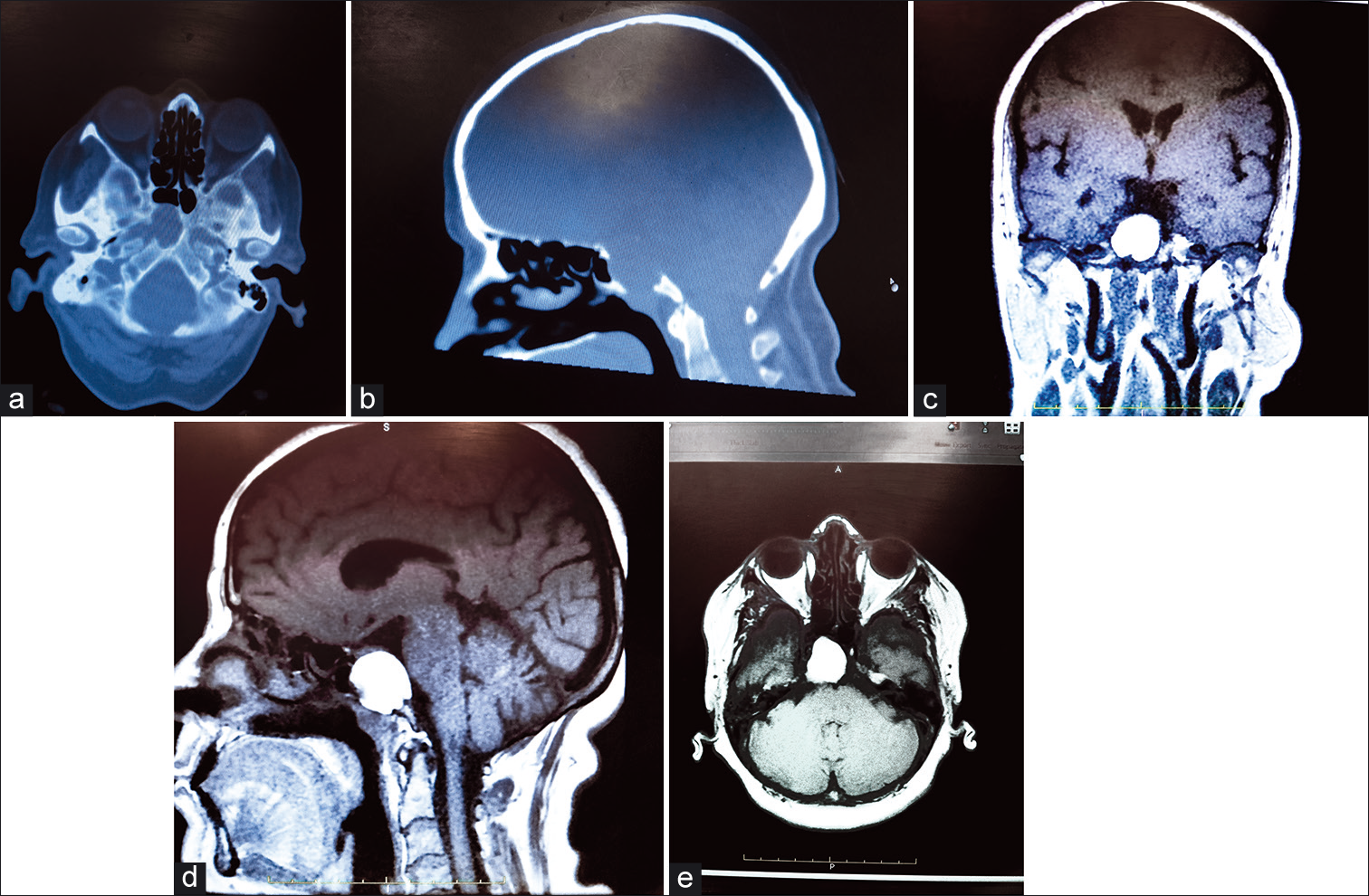
Atypical sellar cyst: A rare case
Date of publication: 20-Jun-2020
Background: Sellar cysts are common in neurosurgery. Around 90% of these are diagnosed as pituitary adenomas. The other 10% are nonadenomatous, inflammatory, infective, metastatic, or cystic in nature. Some rare cysts include dermoid, epidermoid, colloid, and arachnoid. They all have different histological features. The case we present demonstrates a unique cyst with features that are not previously documented.
Risk of fatal sinus arrest induced by low-grade subarachnoid hemorrhage: A case of a young patient with obstructive sleep apnea
Date of publication: 20-Jun-2020
Background: Sleep apnea syndrome (SAS) and subarachnoid hemorrhage (SAH) are both considered possible causes of secondary arrhythmias. However, there are limited reports on the increased risk of bradyarrhythmia for arrhythmia-free SAS patients with SAH.
A spontaneous cervical epidural hematoma mimicking a stroke – A case report
Date of publication: 20-Jun-2020
Background: A spontaneous cervical epidural hematoma (SCEH) is a rare occurrence. It usually presents with quadriparesis, but it may present with hemiparesis or hemiplegia and can easily be misdiagnosed as stroke. We present a case of stroke mimicking SCEH with hemiparesis worsened after tissue plasminogen activator therapy (tPA) followed by emergency cervical decompression laminectomy.