Erratum: Profile of genetic variations in severely calcified carotid plaques by whole-exome sequencing
Date of publication: 13-Mar-2021
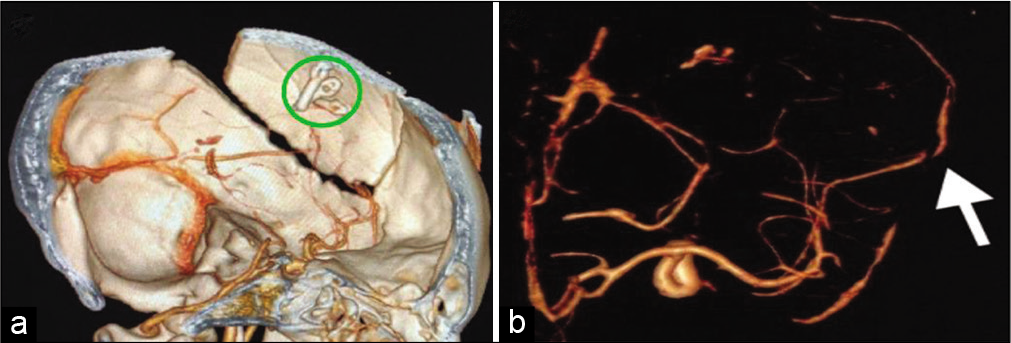
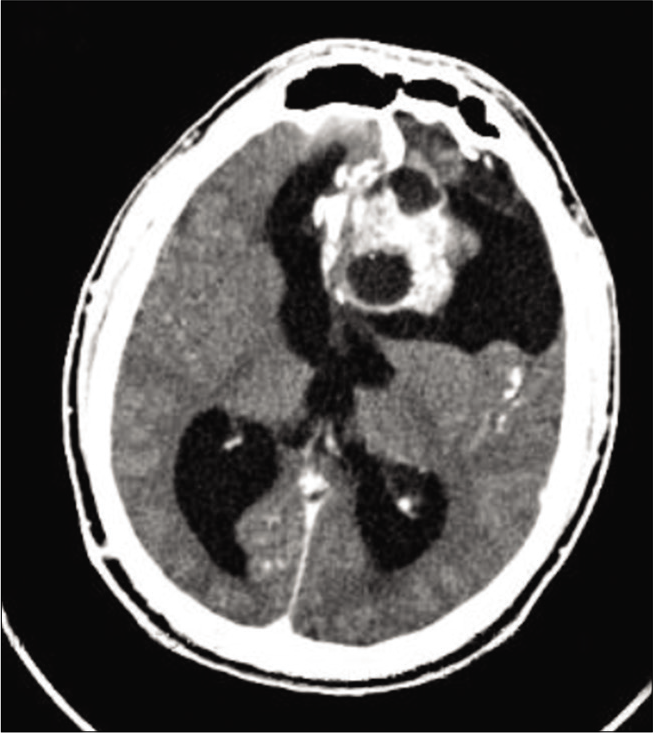
Ruptured giant aneurysm of a cortical middle cerebral artery: A case report
Date of publication: 08-Mar-2021
Background: Aneurysms of the cortical branches of the middle cerebral artery (MCA) are rare. They usually are secondary to traumatic or infectious etiologies and are rarely idiopathic. The specific characteristics of idiopathic aneurysms in such location are not well defined in the literature. The authors report a rare case of a ruptured giant idiopathic cortical MCA aneurysm with review of the available literature on this clinical entity.
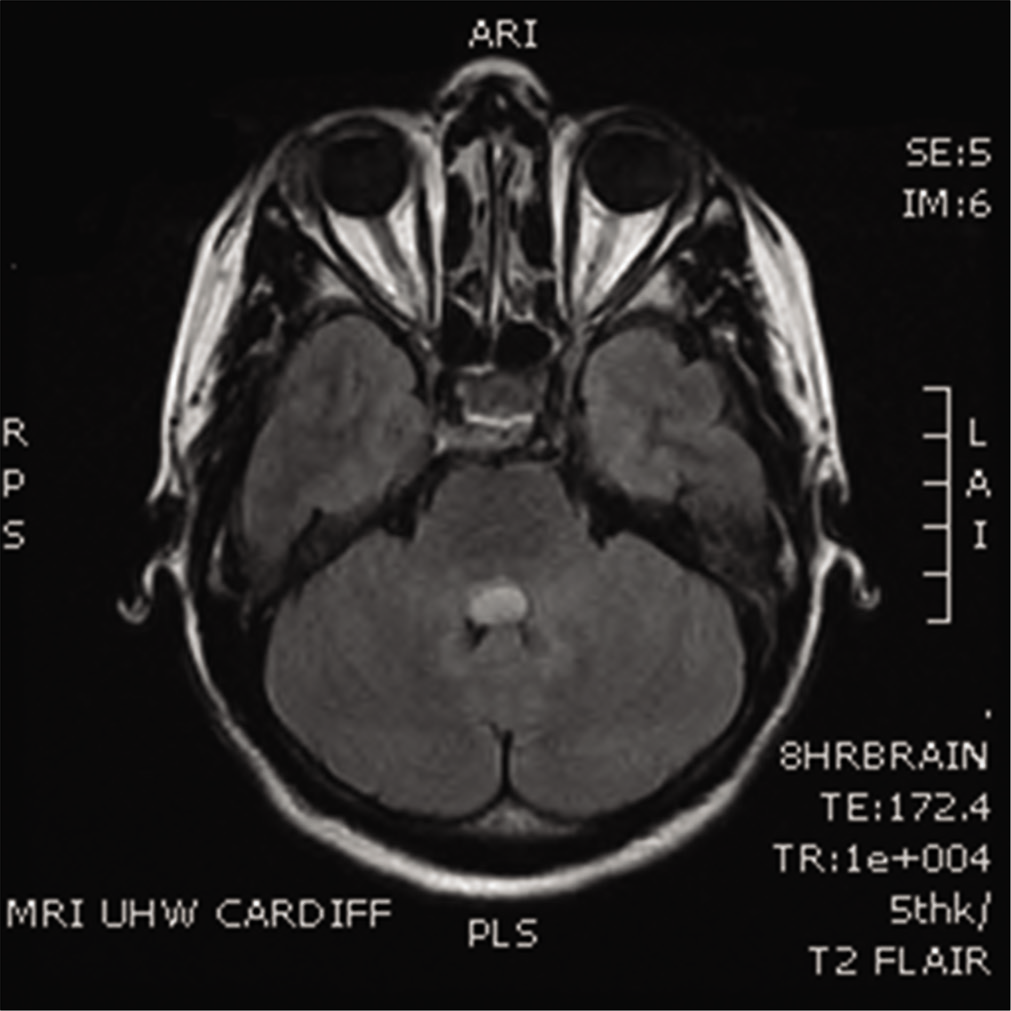
Mollaret’s triangle: An important neuroanatomical territory for all clinicians
Date of publication: 08-Mar-2021
Background: Hypertrophic olivary degeneration is a rare condition caused by damage within the triangle of Guillain and Mollaret. We discuss the anatomical, radiological, and clinical history of this rare condition.
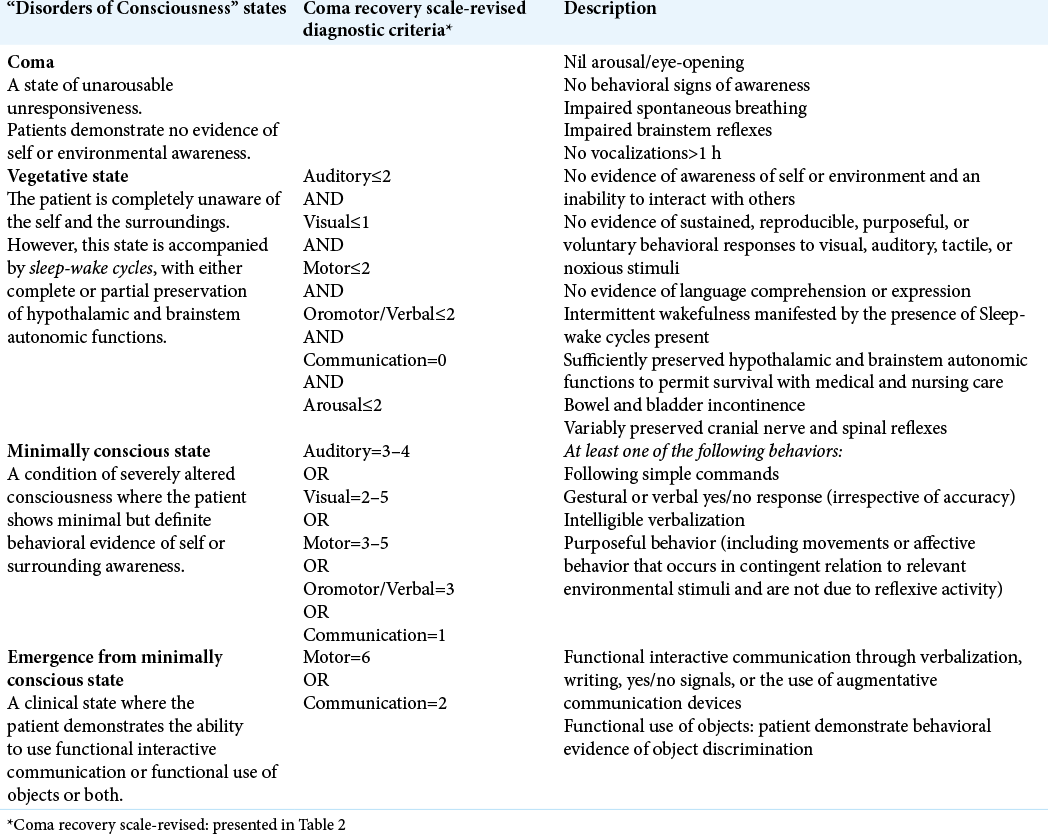
Coma recovery scale: Key clinical tool ignored enough in disorders of consciousness
Date of publication: 08-Mar-2021
Background: Disorders of consciousness (DoC) includes coma, vegetative state (VS), minimally conscious state (MCS), and emergence from the MCS. Aneurysmal rupture with high-grade SAH, traumatic brain injury, and neoplastic brain lesions are some of the frequent pathologies leading to DoC. The diagnostic errors among these DoC are as high as ranging from 25% to 45%, with a probable error in the conclusion of patients’ state, treatment choice, end-of-life decision-making, and prognosis. Some studies also reported that 37–43% of patients were misdiagnosed in VS while demonstrating signs of awareness. Despite its wide acceptance, Coma Recovery Scale-Revised (CRS-r) remained underused or inappropriately utilized, which may lead to substandard or unprofessional patient care. Literature is rare on the knowledge of CRS-r among physicians published from India and across the globe. Therefore, we carried out the present study to ascertain physicians’ knowledge on CRS-r and raise awareness about its justifiable clinical utilization. We also explored the factors associated with this perceived level of experience among participants and recommend frequent physicians’ training for care of patients with DoC.
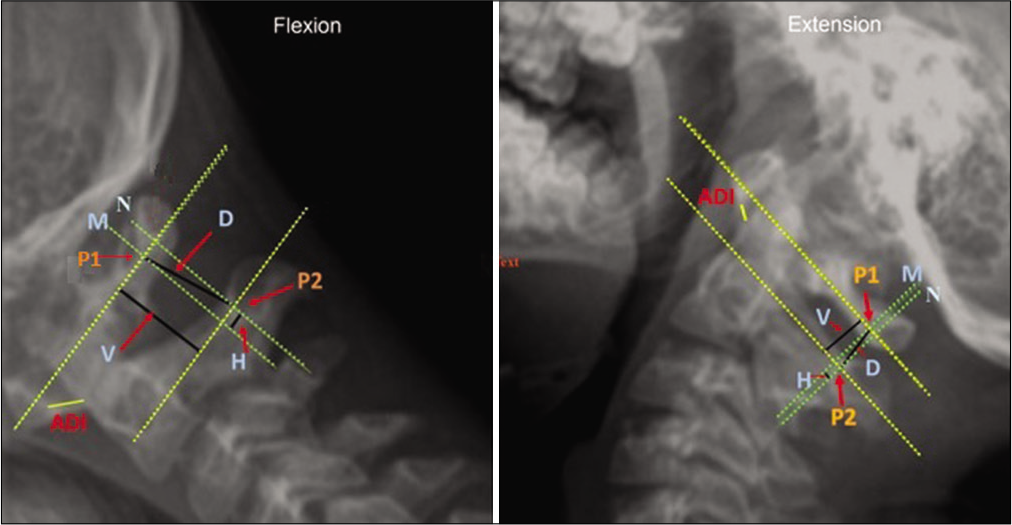
Fiberoptic bronchoscopy versus video laryngoscopy guided intubation in patients with craniovertebral junction instability: A cinefluroscopic comparison
Date of publication: 08-Mar-2021
Background: Manipulation during endotracheal intubation in patients with craniovertebral junction (CVJ) anomalies may cause neurological deterioration due to underlying instability. Fiberoptic-bronchoscopy (FOB) is better than video laryngoscope (VL) for minimizing cervical spine movement during intubation. However, evidence suggesting superiority of FOB in patients with CVJ instability is lacking. We prospectively compared dynamic movements of the upper cervical spine during intubation using FOB with VL in patients with CVJ anomalies.
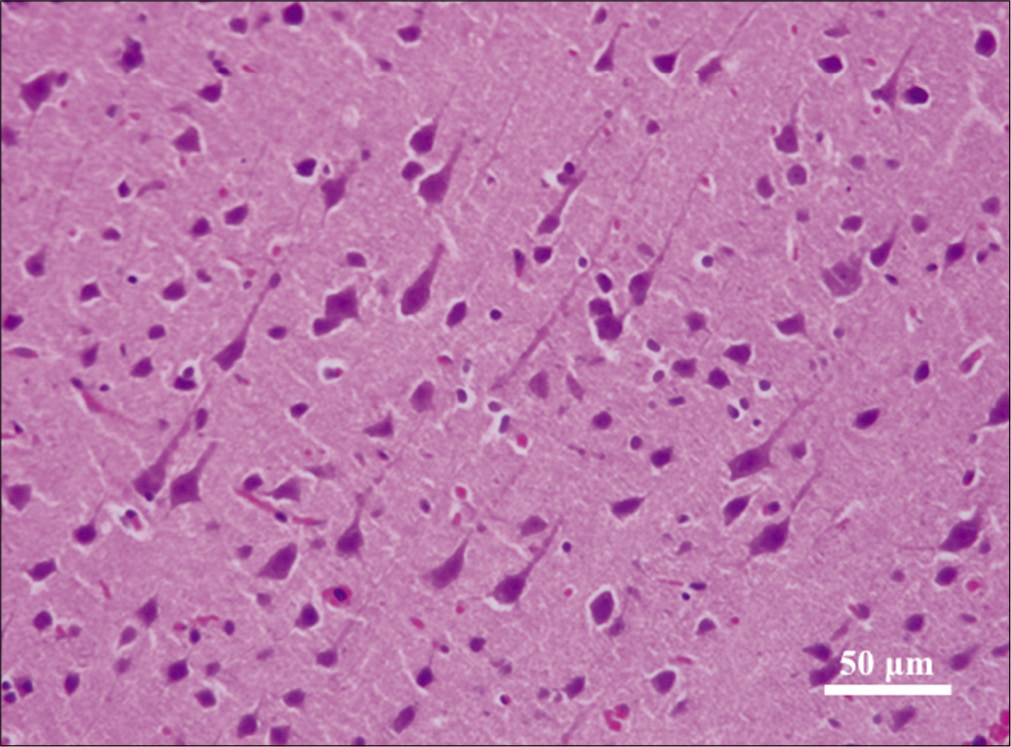
Histopathological changes of neuronal tissue following the use of hydrogen peroxide in neurosurgical procedures
Date of publication: 08-Mar-2021
Background: Hydrogen peroxide (HP) is routinely used in neurosurgical procedures to achieve surgical hemostasis. However, its safety profile is still debatable with various reports depicting range of adverse effects on neuronal tissue. The objective of this paper is to evaluate the safety and efficacy of HP as a hemostatic agent in normal neuronal tissue during neurosurgical procedures conducted on rats.
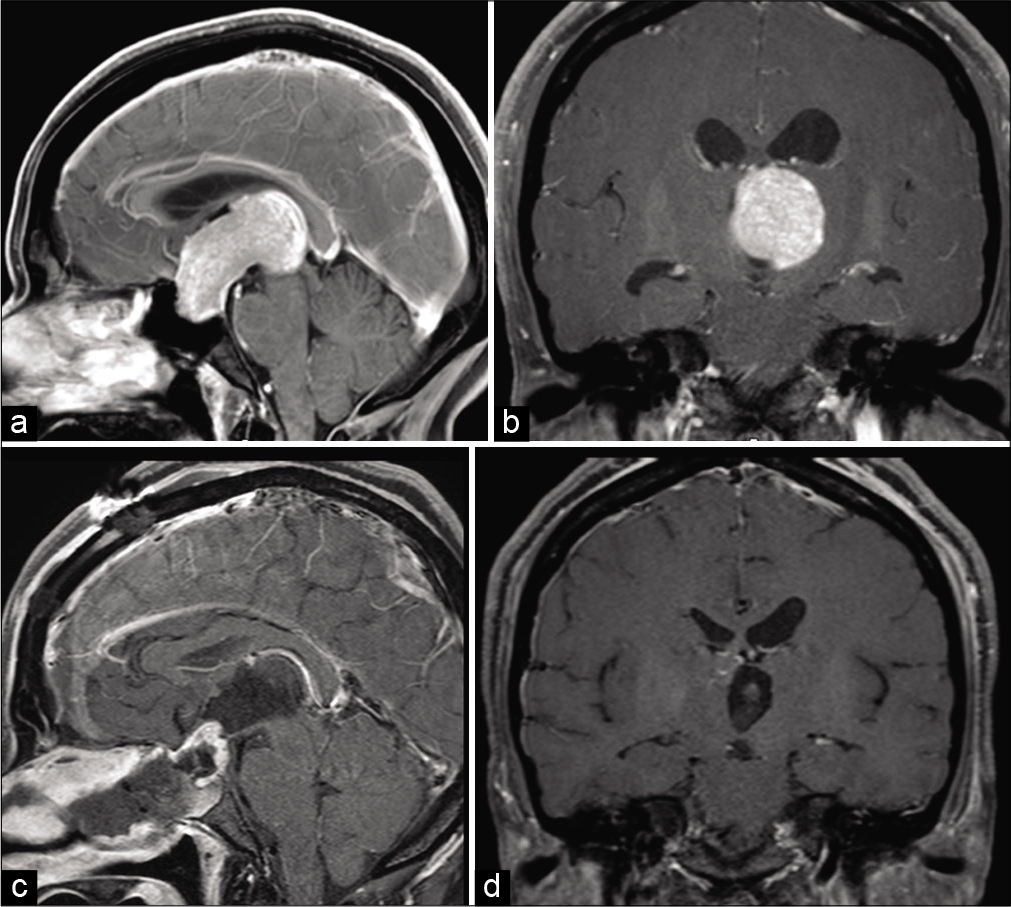
Combined simultaneous endoscopic endonasal and microscopic transventricular surgery using a port retractor system for giant pituitary adenoma: A technical case report
Date of publication: 08-Mar-2021
Background: We report a case of a giant pituitary adenoma with marked extension into the third ventricle that was successfully removed using combined simultaneous endoscopic endonasal surgery (EES) and microscopic transventricular port surgery.
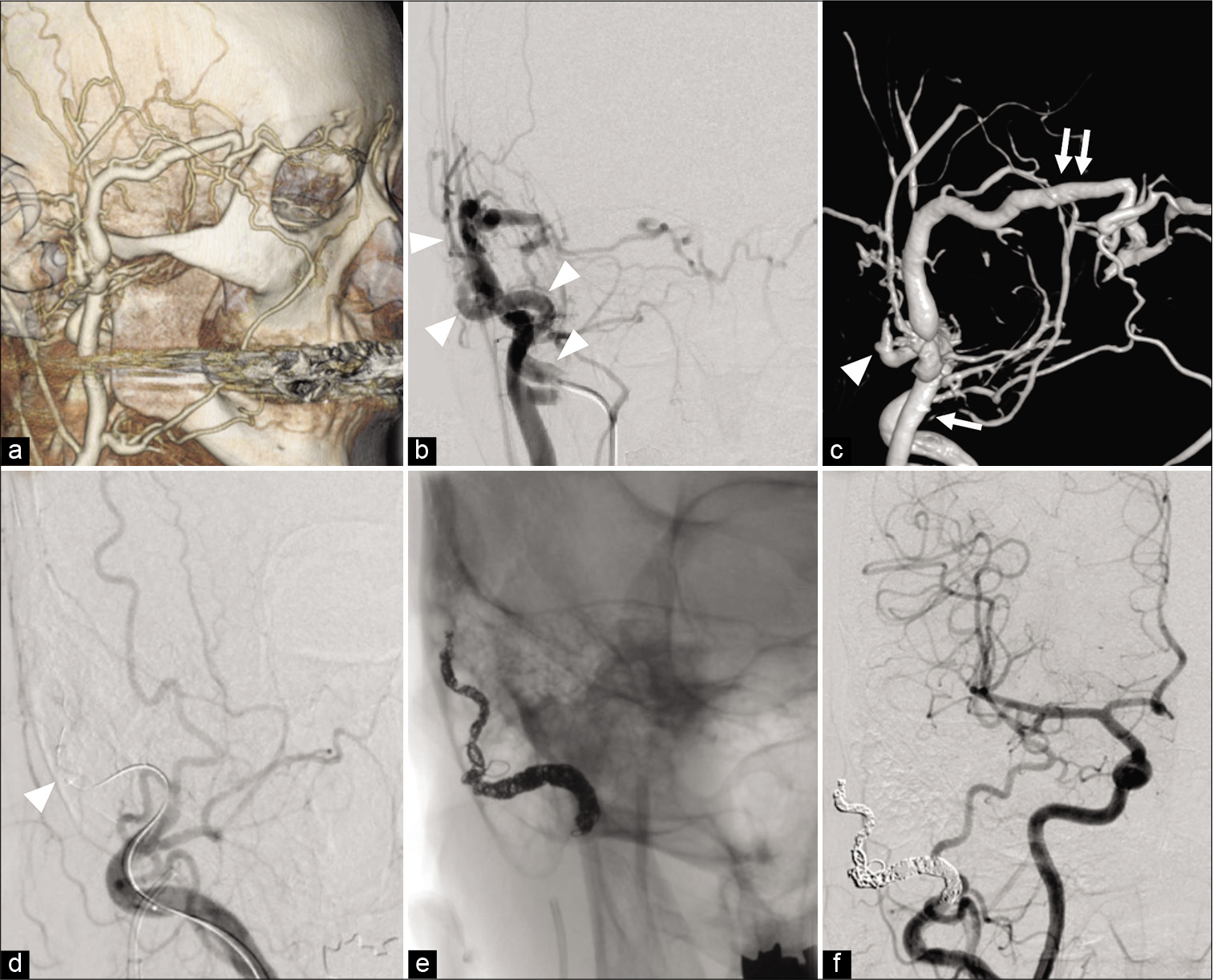
The usefulness of temporary balloon occlusion during transarterial embolization for scalp arteriovenous fistula
Date of publication: 08-Mar-2021
Background: We present two cases of scalp arteriovenous fistula (sAVF) treated by transarterial embolization with the aid of a temporary balloon occlusion (TBO) to detect precise vasculature.
A rare diagnosis of an extraventricular neurocytoma
Date of publication: 08-Mar-2021
Background: Extraventricular neurocytoma (EVN) is an extremely rare neoplasm of the central nervous system. As reported, it arises in a variety of locations, but mainly within the cerebral hemispheres. Despite its histological similarity with central neurocytoma (CN), EVN occurs outside the ventricular system and, in 2007, was recognized by the World Health Organization as a separate entity.
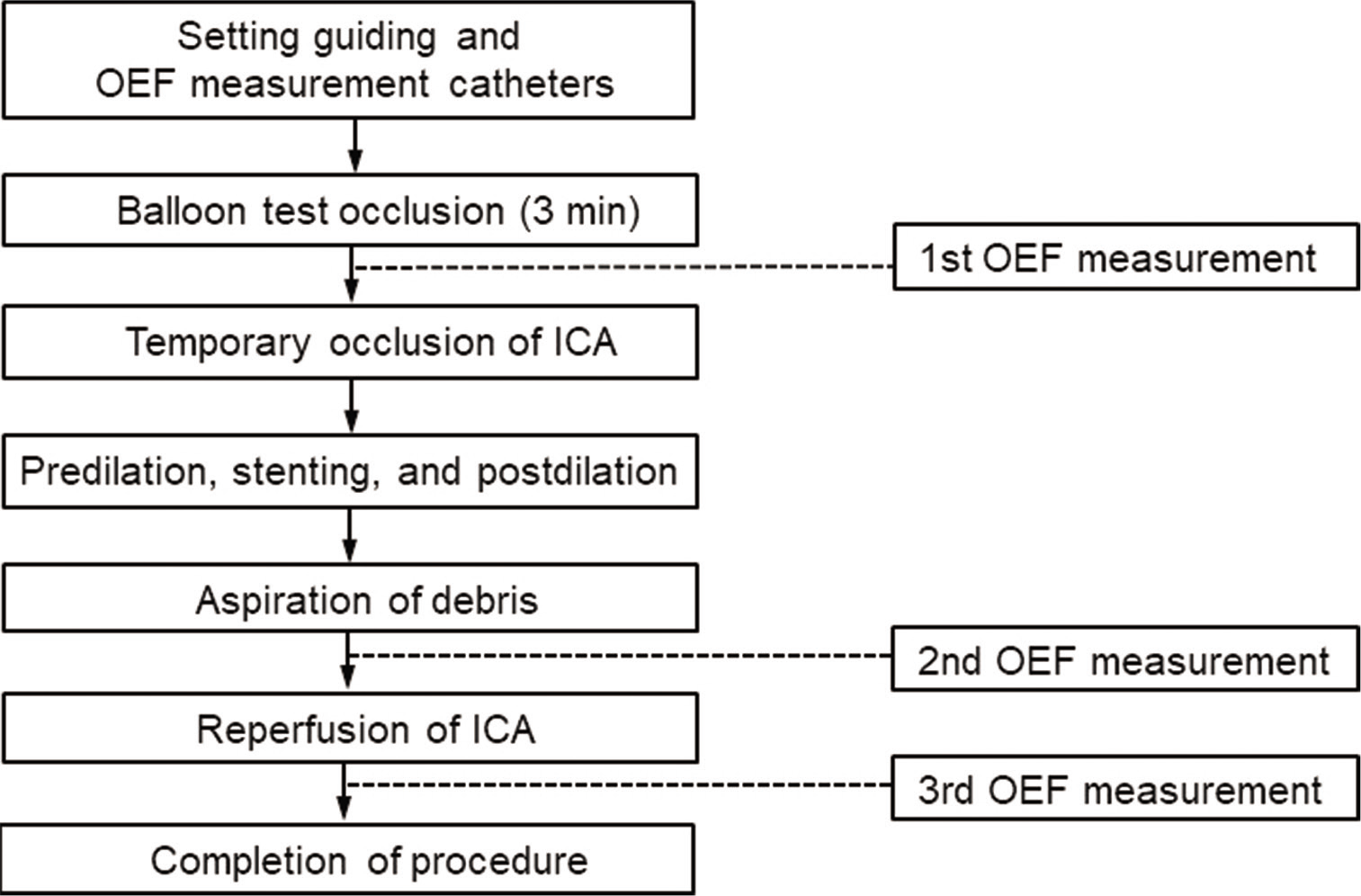
Analysis of postprocedural microembolic infarctions and global oxygen extraction fraction during balloon-protected carotid artery stenting: Preliminary study
Date of publication: 08-Mar-2021
Background: Atherosclerotic carotid stenosis with impaired cerebral perfusion is a risk factor for cerebral ischemia. In major carotid stenoocclusive diseases, increased oxygen extraction fraction (OEF) is associated with ischemic stroke. Balloon-protected carotid artery stenting (CAS) is valuable for high-grade carotid stenosis. However, while balloon-protected CAS can effectively reduce the occurrence of ischemic complications by blocking carotid flow, cerebral hypoperfusion may result in simultaneous cerebral ischemia. We sought to evaluate whether increased OEF during balloon-protected CAS can predict postprocedural microembolic infarction (MI).